Module 8 Intro
| Site: | MoodleHUB.ca 🍁 |
| Course: | Biology 20 SS |
| Book: | Module 8 Intro |
| Printed by: | Guest user |
| Date: | Wednesday, 24 December 2025, 6:52 AM |
Description
Created by IMSreader
Table of contents
- 1. Module 8 Intro
- 1.1. Big Picture
- 1.2. In this Module
- 1.3. Lesson 1 Intro
- 1.4. Page 2
- 1.5. Page 3
- 1.6. Lab
- 1.7. Page 5
- 1.8. Page 6
- 1.9. Page 7
- 1.10. Lesson 2 Intro
- 1.11. Page 2
- 1.12. Lab
- 1.13. Page 4
- 1.14. Page 5
- 1.15. Page 6
- 1.16. Lesson 3 Intro
- 1.17. Page 2
- 1.18. Page 3
- 1.19. Page 4
- 1.20. Page 5
- 1.21. Lab
- 1.22. Page 7
- 1.23. Page 8
- 1.24. Page 9
- 1.25. Lesson 4 Intro
- 1.26. Page 2
- 1.27. Page 3
- 1.28. Page 4
- 1.29. Page 5
- 1.30. Lesson 5 Intro
- 1.31. Page 2
- 1.32. Page 3
- 1.33. Page 4
- 1.34. Page 5
- 1.35. Lesson 6 Intro
- 1.36. Page 2
- 1.37. Page 3
- 1.38. Page 4
- 1.39. Page 5
- 1.40. Lesson 7 Intro
- 1.41. Page 2
- 1.42. Page 3
- 1.43. Page 4
- 1.44. Lesson 8 Intro
- 1.45. Page 2
- 1.46. Page 3
- 1.47. Page 4
- 1.48. Page 5
- 1.49. Lesson 9 Intro
- 1.50. Page 2
- 1.51. Lab
- 1.52. Page 4
- 1.53. Page 5
- 1.54. Page 6
- 1.55. Module Summary/Assessment
- 1.56. Module Glossary
1. Module 8 Intro
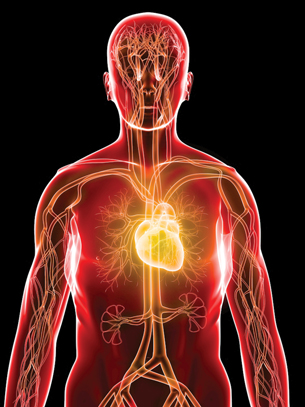
Module 8—Circulation, Immunity, and Excretion
Module Introduction
In this module you will study the circulatory system, the lymphatic system, the immune system, and the excretory system. Blood is a multifaceted fluid that transports material, clots after injuries, and provides a defence against invading pathogens. It also aids in maintaining fluid balance and temperature homeostasis. You will learn about T-cells, B-cells, and antibodies, which are all components of the defence system of the human body.
As well, you will gain an understanding of the ABO and Rh blood types. You will explore how the kidneys filter blood, reabsorb substances for reuse, and secrete excess or toxic substances as urine.
You no doubt have had direct physical experience with these systems. If you have ever skinned your knee or cut your finger, you have seen first hand what blood looks like. You may have noticed that blood gushed from your wounds, slowed, and finally clotted to reclose the break in the circulatory system. The injury may have become sore and infected, but thanks to your immune system with its specialized white blood cells in your blood, an attack on invading germs prevented any greater damage.
In this module you will have the opportunity to investigate the function of specialized structures and their role in biochemical homeostasis. As you study each system, you will be introduced to various technologies used to solve problems involving dysfunctions and disorders of each system. You will explore this question: How do the circulatory, immune, and excretory systems maintain life-sustaining internal equilibrium through matter and energy exchange?
By the end of this module you will have completed activities that are to be marked by your teacher and some that help to build confidence in your ability to understand, interpret, and express key course concepts. Everything should be saved in your course folder. At some point you may need to review pieces of information for exams, project work, or discussions.
For example, you will need to complete a unified response on a muscle disorder for your module project and will need to use information gathered throughout this module. When you are ready to complete the module project, you will find the project description in the Module Summary.
1.1. Big Picture
Module 8—Circulation, Immunity, and Excretion
 Big Picture
Big Picture

© Tomasz Szymanski/shutterstock
When you turn on the tap to fill a glass with water to drink, do you ever stop to consider how that water was circulated, filtered, and purified of water-borne parasites to make it safe to drink? Or do you just take it for granted that there is a process the water goes through to end up in your glass?
For that matter, you probably also take it for granted that your body has a way to filter, purify, and circulate blood, remove wastes, and has a system to protect you from being sick all the time.
Many parallels can be drawn between a water treatment plant and human body systems in relation to circulation, immunity, and excretion.

© Sebastian Kaulitzki/shutterstock
The closest parallel would be the function of filtration. Water moves through a series of processes that filter out contaminants. Clean water is reintroduced to the environment. Wastes are collected and stored until they can be disposed. Similarly, blood moves through millions of filtering structures within the kidney. Once toxins and metabolic wastes are removed, filtered blood is reabsorbed and continues on its journey to the rest of the body. Waste, in the form of urine, is collected by the bladder and excreted.
Another parallel can be made between a water treatment plant and the circulatory system. A sophisticated network of pipes and valves control the movement of natural water which may be contaminated into a treatment plant and clean water back out to the environment. In humans, a complex network of blood vessels move oxygenated and deoxygenated blood to and from the heart. The heart, which is a powerful pump containing a series of valves, sets the rhythm for the movement of blood.
Finally, a parallel can be drawn between the processes involved in treating the water in a water treatment plant and the immune system. As water moves through a treatment plant, substances and living organisms are added to the water to rid it of biological contaminants. In the body, different types of cells are produced which interact with foreign substances. The foreign substances are then dissolved and reabsorbed or filtered out by the kidneys.
As in the human body, all parts of a water treatment plant work together to support function and a balanced system.
In this module you will explore this question: How do the circulatory, immune, and excretory systems maintain internal equilibrium through matter and energy exchange?
As you work through this module you will explore the following essential questions:
- What are the major structures and functions of the circulatory, immune, and excretory systems?
- How do the principle structures of the circulatory system move blood through the body?
- What is the relationship between blood pressure, heart rate, and exercise?
- How can technology treat disorders of the circulatory, immune, and excretory systems?
- What are the main components of blood, and how do they look under a microscope?
- How does blood help to regulate body temperature?
- At the capillary level, how does the circulatory system aid the digestive, excretory, respiratory, and motor systems’ exchange of matter with the environment?
- How do the cellular and non-cellular components of the human defense system work together to maintain homeostasis?
- How do antigens identify blood types and Rh factors?
- How does the nephron function in maintaining the composition of blood plasma?
- How do the kidneys function in excreting metabolic wastes and expelling them into the environment?
- How do the kidneys contribute to homeostasis in terms of water and ions?
- How does the design of the kidney relate to dialysis technologies?
In addition to the lesson assignments and labs, there will be a module project to complete. For the module project you will have the choice between three extended responses. The purpose of an extended response is to help you take a closer look at a specific area of study. In the module project you will choose between investigating the heart, an immune response, or a disease of the kidney.
When you are ready for more information about the project, go to the Module Summary for instructions.
1.2. In this Module
Module 8—Circulation, Immunity, and Excretion
In This Module
Lesson 1—Structures of the Circulatory System
Pumps, valves, and pipes sound very mechanical. However, the organic version of pipes, pumps, and valves are what the human body depends on for the transport of blood, nutrients, and wastes.
- What are the major structures and functions of the circulatory system?
- How do the principal structures of the circulatory system move blood through the body?
Lesson 2—Investigating the Circulatory System
Heart rate and blood pressure are two easily measured vital statistics. These measurements are related to your overall physical health. Sometimes people experience problems with their circulatory system, which weakens their overall health. Technology has been developed to help deal with such problems.
- What is the relationship between the heart rate, blood pressure, and exercise?
- How can technology treat disorders of the circulatory system?
Lesson 3—Blood
Water is an essential component of the biosphere. Meanwhile, blood is an essential component of the human body. Blood is a fluid suspension as well as a solvent. Each part of the suspension serves a purpose while substances dissolve into blood to be transported, similar to the role of water in the biosphere. Blood also regulates body temperature based on the property of water that allows water to also regulate climate (specific heat capacity) and the heat exchange system that is installed in all humans.
- What are the main components of blood? How do these components contribute to transporting, clotting, and resisting the influence of pathogens?
- How does blood help to regulate body temperature?
Lesson 4—Circulation
A complex network of piping moves water through the different processes of water treatment. The movement of water is dependent on pressure and concentration gradients. In humans, billions of capillaries deliver nutrients and remove wastes based on pressure and concentration gradients.
- At the capillary level, how does the circulatory system aid the digestive, excretory, respiratory, and motor systems’ exchange of matter with the environment?
Lesson 5—The Lymphatic System and Immunity
How does your body try to guard you from illness? Sometimes you do get sick. However, considering the millions of bacteria and viruses that you come into contact with on a daily basis, your body does a relatively good job of warding off serious infection.
- What is the function of the lymphatic system?
- How do the cellular and non-cellular components of the human defense system work together to maintain homeostasis?
Lesson 6—Blood Types and Rh Factors
What’s your type? Understanding that not all blood is the same is important in case of an emergency where you may require a blood donation. There are specific reasons why your body won’t accept blood from just anyone.
- How do antigens identify blood types and Rh factors?
Lesson 7—Structures and Functions of the Excretory System
Why do people urinate? This lesson is an introduction to the structures involved in urination as well as an introduction to the structures that coordinate the complex filtration of blood and maintain fluid and salt levels.
- What are the principal structures of the excretory system, and how do they function?
- How do nephrons contribute to the function of the excretory system?
Lesson 8—Urine Formation in the Nephron
Urine is formed by the body as a way to maintain homeostasis. Wastes are released in urine and the kidneys ensure that proper levels of solutes are present in the blood plasma.
- How does the nephron function in maintaining the composition of blood plasma?
- How do the kidneys function in excreting metabolic wastes and expelling them into the environment?
Lesson 9—Maintaining the Excretory System
The main role of the excretory system is to filter nutrients from waste, reabsorb water, and maintain critical electrolyte levels. Sometimes kidneys become damaged and people may need to undergo dialysis to filter their blood.
- How do the kidneys contribute to homeostasis in terms of water and ions?
- How does the design of the kidney relate to dialysis technologies?
1.3. Lesson 1 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 1—Structures of the Circulatory System
 Get Focused
Get Focused

© Krzysztof Slusarczyk/shutterstock
The circulatory system of a water treatment plant is based upon pumps, closed tubular structures or pipes, and valves. Much like water is moved through a water treatment plant, the human body has a strong central pump , pipes of various sizes (blood vessels), and valves (heart and veins) that work to move blood (nutrients, gases, wastes) through the body.
In this lesson you will learn about the heart’s structure and function. You will examine its role in circulating blood throughout the body. You will also learn about the blood vessels that lead to and from the heart.
In this lesson you will explore the following essential questions:
- What are the major structures and functions of the circulatory system?
- How do the principal structures of the circulatory system move blood through the body?
 Module 8: Lesson 1 Assignment
Module 8: Lesson 1 Assignment
Your teacher-marked Module 8: Lesson 1 Assignment requires you to submit a response to the following:
- Lab: Investigation 8.A: Identifying Structures of the Circulatory System
You can access your Module 8: Lesson 1 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
1.4. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Watch and Listen
Watch and Listen
Major Components of the Circulatory System
Before you begin this lesson, read the bottom of page 268 in your textbook.

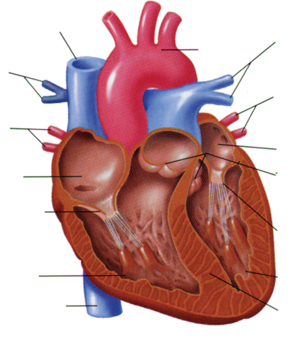
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 269, fig. 8.2. Reproduced by permission.
Watch this animation. It shows both the heart’s structure and the blood flow through its chambers and associated blood vessels. The movement of blood through the heart is referred to as the cardiac cycle. As in the previous diagram of the heart, the right-hand side of your heart is referred to as left. It’s like you are facing someone else and looking at this person’s heart. As you are watching, take note of the heart’s division into two distinct sides.
The right side contains deoxygenated blood received from the body and is pumped from the heart toward the lungs. The left side contains oxygenated blood from the lungs, which is pumped out to supply the body’s tissues.
atria: one of the two upper chambers of the heart that collects blood flowing into the heart
The right atrium receives blood from systemic circulation, and the left receives blood from pulmonary circulation.
atrioventricular valve: a membranous extension of a vessel or the heart wall that opens and closes, ensuring one-way fluid flow; located between the atrium and ventricle
ventricle: one of the two lower chambers of the heart; each ventricle receives blood from one of the atria and pumps it into systemic or pulmonary circulation
Recognize that blood flows simultaneously into the top two chambers of the heart (the atria). The atria contract in unison to pass blood through the atrioventricular valves (more commonly referred to as A-V valves) and then pass blood into the ventricles. The ventricles also contract synchronously to push blood from the heart.
1.5. Page 3
Module 8—Circulation, Immunity, and Excretion
 Read
Read
Why Does the Heart Pump Rhythmically?
A healthy heart beats steadily and rhythmically at a rate of about 60 to 100 beats per minute when at rest (normal sinus rhythm). During strenuous exercise, the heart can increase the amount of blood it pumps up to four times the amount it pumps at rest, within only a matter of seconds. As a specialized organ, the heart depends on specialized muscle cells and fibres to pump in a coordinated, rhythmic fashion.
endocardium: the innermost layer of tissue that lines the chambers of the heart
This sheet of shiny, white tissue also lines the body’s blood vessels to help form a continuous lining through the circulatory system. This lining helps blood flow smoothly and prevents the formation of clots.
myocardial fibres: a specialized cardiac muscle that can contract as well as conduct electrical impulses; not found anywhere else in the body
Purkinje fibres: specialized fibres that transmit electrical impulses to the cardiac muscles in the heart to induce rhythmic muscle contraction
The pumping action (muscle contraction/relaxation) is coordinated by Purkinje fibres (or Purkyne tissue) located in the inner ventrical walls of the heart, just beneath the endocardium or lining of the heart chambers. These fibres are specialized myocardial fibres that conduct an electrical stimulus or impulse that enables the heart to contract in a coordinated fashion.
Read more about “The Beating Heart” on pages 272 to 274 of the textbook or watch this animation.

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 274, fig. 8.7. Reproduced by permission.
Systemic vs Pulmonary Circulation
pulmonary: having to do with the lungs
systemic: a body system in general
It is important to distinguish between pulmonary circulation and systemic circulation. Pulmonary circulation occurs when the right side of the heart pumps deoxygenated blood to the lungs via the pulmonary arteries. Pulmonary veins bring oxygenated blood back to the left side of the heart to be distributed to the rest of the body through the arteries. In the pulmonary system, arteries carry deoxygenated blood and veins carry oxygenated blood.
This is different from systemic circulation. Systemic circulation involves the circulation of blood to all other parts of the body aside from the lungs. This is the portion of the cardiovascular system that carries oxygenated blood away from the heart, to the body, and then returns deoxygenated blood back to the heart.
Read pages 268 to 270 in the textbook to obtain more details about the structure and function of the heart.
1.6. Lab
Module 8—Circulation, Immunity, and Excretion
 Lab: Investigation 8.A: Identifying Structures of the Circulatory System
Lab: Investigation 8.A: Identifying Structures of the Circulatory System

You now have the opportunity to dissect a heart. You may choose to do a real dissection, or you may choose to view a virtual dissection. If you perform a real dissection you will need to follow the steps outlined in Investigation 8.A on page 272 of the textbook.
Otherwise, view the following slide show of the dissection of a sheep’s heart to help you identify structures. The show will also help you fully understand how oxygenated and deoxygenated blood moves through the heart to the rest of the body. Sheep have a four-chambered heart, just like humans, and a sheep’s heart is similar in size. By studying the anatomy of a sheep's heart, you can learn about how your own heart pumps blood through your body and keeps you alive.
Once you have completed the dissection of your choice, go to the Lesson 1 Assignment to finish an activity charting the flow of blood through the principal structures of the human heart.
1.7. Page 5
Module 8—Circulation, Immunity, and Excretion
 Read
Read
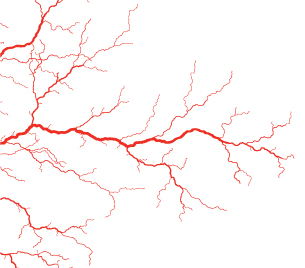
The Structure of Blood Vessels
© Sebastian Kaulitzki/shutterstock
Arteries carry oxygen-rich blood away from the heart, except for the pulmonary arteries. These arteries carry deoxygenated blood from the heart to the lungs. Veins carry oxygen-poor blood toward the heart, except for pulmonary veins. There are four pulmonary veins and they carry oxygen-rich blood from the lungs to the left atrium. Just remember, the pulmonary arteries and veins carry the opposite kind of blood to the rest of the arteries and veins in the body.
Blood travels from arteries to capilliaries. Capillaries are very thin and fragile. They are actually only one red blood cell thick and are the blood vessels that network throughout your entire body. The arteries deliver the oxygen-rich blood to the capillaries, where the actual exchange of oxygen and carbon dioxide occurs. The capillaries then deliver the waste-rich blood to the veins for transport back to the lungs and heart. Nutrients, gas, and other materials are transported into and out of the capilliaries, depending if they are necessary reactants or waste products of metabolism.

© TAOLMOR/shutterstock
Systemic circulation moves in the following cycle:
heart → arteries → body tissue capillaries → veins → heart
Continue learning about blood vessels by reading pages 270 and 271 of the textbook.
 Self-Check
Self-Check
SC 1. What blood vessels carry blood away from the heart?
SC 2. What blood vessels carry blood to the heart?
SC 3. Compare the structures of the three types of blood vessels.
 Self-Check Answers
Self-Check Answers
SC 1. Arteries carry blood away from the heart.
SC 2. Veins carry blood to the heart.
SC 3. Veins are not elastic and require valves to move blood back to the heart. Otherwise, blood would pool in the extremities. Arteries are elastic so they can expand with the force of blood as it pumps from the heart. Arteries expand as ventricles relax and keep the blood flowing. Capillaries are very small and spread out in a network that allows single blood cells to be exposed to individual cells.
1.8. Page 6
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect
Reflect and Connect
 Self-Check
Self-Check
SC 4. Using “Figure 8.2” on page 269 from the textbook, label the external and internal views of the heart. You can visualize or write down the labels. Choose what works best for you.
- External View of the Heart

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 269, fig. 8.2. Reproduced by permission.
- Internal View of the Heart
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 269, fig. 8.2. Reproduced by permission.
 Module 8: Lesson 1 Assignment
Module 8: Lesson 1 Assignment
Remember to submit the Assignment answers to your teacher as part of your Module 8: Lesson 1 Assignment.
1.9. Page 7
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following essential questions:
- What are the major structures and their functions of the circulatory system?
- How do the principal structures of the circulatory system move blood through the body?
The human circulatory system is made up of the heart, blood vessels, and blood. The heart is a muscular pump with two atria that receive blood from the vena cava and pulmonary vein.
Deoxygenated blood from the vena cava collect in the right atrium, while oxygenated blood from the pulmonary vein collects in the left atrium. The right atrioventricular valve opens to move deoxygenated blood into the right ventricle. Simultaneously, the left atrioventricular valve opens to move oxygenated blood into the left ventricle.
The pumping action (muscle contraction/relaxation) is coordinated by Purkinje fibres in the septum. Nodes in the right atrium conduct electrical impulses to these fibres, which induce rhythmic muscle contraction. This give a “lub dub” sound to the blood moving through the chambers of your heart.
From the ventricles, semilunar valves open and close at the pulmonary artery trunk and aorta trunk. Deoxygenated blood moves from the right ventricle to the lungs, while blood that has returned oxygenated from the lungs is pumped through the aorta.
Arteries such as the aorta take blood away from the heart. Veins, such as the vena cava and pulmonary vein, return blood to the heart. Blood moves from arteries to capillaries to engage in energy and matter exchange. Blood moves from the capillaries to the veins, and blood is moved back to the heart to be reoxygenated.
Lesson Glossary
endocardium: the innermost layer of tissue that lines the chambers of the heart
This sheet of shiny white tissue also lines the body’s blood vessels to help form a continuous lining through the circulatory system. This lining helps blood flow smoothly and prevents the formation of clots.
myocardial fibres: a specialized cardiac muscle that can contract as well as conduct electrical impulses; not found anywhere else in the body
pulmonary: having to do with the lungs
Purkinje fibres: specialized fibres that transmit electrical impulses to the cardiac muscles in the heart to induce rhythmic muscle contraction
systemic: a body system in general
1.10. Lesson 2 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 2—Investigating the Circulatory System
 Get Focused
Get Focused

© Oguz Aral/shutterstock
What happens when a valve won’t open or a pump fails in a water treatment plant? Water is diverted through alternative systems—a backup valve opens or a pump works extra hard to keep up with the demands of regulating water flow. Humans put strain on their systems when they exercise or if they have some kind of disorder. The heart must keep up with changes in the internal environment.
One way of improving a system is to fix or replace a pump. This is easy enough to do in a mechanical system. You turn a valve off, fix or replace the pump, and open the valve to resume the flow. In the human system, heart transplants have become an option where the organ is failing. However, this option has serious risks and limitations.
Many new technologies have been developed to treat heart disease or correct congenital defects. These changes have allowed many people to live with a more efficient circulatory system. Regular exercise and healthy living can be the best way to prevent heart disease and help your body maintain homeostasis.

© Tony Robinson/shutterstock
In this lesson you will explore the following essential questions:
-
What is the relationship between the heart rate, blood pressure, and exercise?
-
How can technology treat disorders of the circulatory system?
 Module 8: Lesson 2 Assignment
Module 8: Lesson 2 Assignment
Your teacher-marked Module 8: Lesson 2 Assignment requires you to submit a response to the following:
-
Lab: Virtual Blood Pressure
-
TR 1. Heart Rate Recovery
You can access your Module 8: Lesson 2 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all the questions and place those answers in your course folder.
1.11. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Watch and Listen
Watch and Listen
As a review, watch this animation about the role of pressure in the beating heart.
 Read
Read
Blood Pressure
arterial pressure: the pressure blood exerts on artery walls
sphygmomanometer: a device used to measure blood pressure
diastole: the relaxation of the heart
systole: contraction of the heart
stethoscope: an acoustic medical device designed to listen to internal sounds of the human body
Have you ever been in a drugstore and decided to try sticking an arm in the blood-pressure machine by the pharmacy? A person of average height and weight typically gets a reading close to 120/80. What do these numbers mean? How can these numbers be a measure of your health?
Blood pressure refers to the force exerted by circulating blood on the walls of blood vessels. It, along with your pulse, make up the vital signs. The pressure of the circulating blood decreases as blood moves through arteries, veins, and capillaries; the term blood pressure generally refers to arterial pressure. Using a blood-pressure cuff, or sphygmomanometer, the pressure in an artery of your arm is measured.
Blood pressure is composed of two measurements: diastole and systole. Systolic pressure is the measurement of peak pressure in an artery at the beginning of the cardiac cycle or during ventricular contraction. Diastolic pressure is the measurement of the lowest pressure during the resting phase of the cardiac cycle or during ventricular relaxation. A blood-pressure reading is given by the ratio of systole over diastole.

© Lloyd Paulson/shutterstock
How do doctors know your blood pressure? If you can recall a visit to the doctor where you have had your blood pressure taken, a cuff is normally fastened firmly around your upper right arm at roughly the same height as your heart. You are seated with your arm supported by the doctor. The cuff is inflated by pumping a small rubber bulb until the artery in your arm is completely blocked. Listening with a stethoscope to the artery at your elbow, your doctor slowly releases the pressure in the cuff. As the pressure in the cuffs falls, a "whooshing" or pounding sound is heard to indicate that the blood flow has started again in the artery. The pressure at which the whoosing sound began is noted by your doctor.
An older method, which is still used today, has the cuff attached to a measuring unit on the wall and the doctor reads the height (mm) of mercury and records this number as the systolic pressure. Newer cuffs have a pressure gauge built in or are digital. The cuff pressure is further released until the whooshing sound can no longer be heard, and this is recorded as diastolic blood pressure.
What do the blood-pressure readings mean?
High Blood Pressure Range
Systolic pressure (mm Hg) |
Diastolic pressure (mm Hg) |
Stages of High Blood Pressure |
210 |
120 |
Stage 4 |
180 |
110 |
Stage 3 |
160 |
100 |
Stage 2 |
140 |
90 |
Stage 1 |
Average Blood Pressure Range
Systolic pressure (mm Hg) |
Diastolic pressure (mm Hg) |
Pressure Range |
130 |
85 |
High Average Blood Pressure |
120 |
80 |
Average Blood Pressure |
110 |
75 |
Low Average Blood Pressure |
Low Blood Pressure Range
Systolic pressure (mm Hg) |
Diastolic pressure (mm Hg) |
Pressure Range |
90 |
60 |
Borderline Low Blood Pressure |
60 |
40 |
Too Low Blood Pressure |
50 |
33 |
Dangerously Low Blood Pressure |
An average reading means that, in terms of your circulatory system, you are in relatively good circulatory system health. High or low blood pressures can indicate that some system in your body, possibly the circulatory system, is impaired and unable to maintain homeostasis. In the following activity you will explore factors that cause high blood pressure known as hypertension.
1.12. Lab
Module 8—Circulation, Immunity, and Excretion
Lab: Virtual Blood Pressure
In this investigation you will use a virtual lab to determine what factors affect the likelihood of hypertension. You will investigate the effect of age and gender on group blood pressure averages.
Once you have entered the virtual lab, notice the Purpose and Objectives. You will record these on your Lesson 2 Assignment. Follow the steps of Procedure. You will have a room full of virtual test subjects, all with different lifestyles and medical histories. Based on what information you record, you will make conclusions about what factors you think contribute to high blood pressure.
You will include the following items in your Lesson 2 Assignment:
- data tables
- graphs
- a sample set of calculations
- responses to three journal questions
- lab conclusions
Your Module 8: Lesson 2 Assignment will give you further instructions.
1.13. Page 4
Module 8—Circulation, Immunity, and Excretion
 Read
Read
Heart Rate
Heart rate is the number of times your heart beats in a minute. Average resting heart rates are around 70 beats/min. On average, your heart (a fist-sized organ) will beat close to three billion times over a lifetime. More than 200 million litres of blood will pass through its chambers.

Courtesy of Benutzer Hase
World-class cyclists like Tour de France champion Lance Armstrong and Canadian olympic gold medallist Lori-Ann Muenzer are among the fittest athletes on the planet. They have incredibly low resting heart rates of 20 to 30 beats per minute. In order to meet the demands of their grueling sport, they need to have extremely powerful hearts. How do they achieve this?
Your heart is a muscle. As you learned in Module 6, muscles can be made stronger through repeated activity that stimulates the growth of muscle fibres. How can you strengthen your heart muscle? You can participate in activities that increase your heart rate such as running, aerobics, weight training, or any activity that increases cellular respiration rates (increased oxygen demands to provide energy from oxidizing glucose).
These activities will make the heart beat faster, meaning that it will relax and contract at quicker intervals to increase the rate of circulation. Cell demands for oxygen and rising levels of carbon dioxide also stimulate a faster heart rate as the body responds to a change in its environment. Meanwhile, the extra contraction of the heart serves to increase its strength and its overall efficiency.
This means that with each contraction, a stronger heart will move more blood. Think of an air mattress pump—if you push the pump weakly, it will take twice as much energy and pumping to fill up the air mattress. If you use strong pushes of the pump, the air mattress is filled more quickly and with less effort. In much the same way, a strong heart pumps more blood with each contraction. A strong heart does not have to contract as often in order to circulate blood. This results in a lower heart rate and a greater work capacity.

© Julien Tromeur/shutterstock
Due to intense cardiovascular training schedules, elite athletes such as Lance Armstrong work at creating the most efficient work output with the least amount of energy. They achieve such low resting heart rates due to the strength of muscle in their heart developed as a result of rigorous cardiovascular activities.
Read pages 275 and 276 of the textbook to learn more about the effects of exercise on the heart.
 Self-Check
Self-Check
SC 1. What is the relationship between heart rate and blood pressure?
 Self-Check Answer
Self-Check Answer
SC 1. High blood pressure is linked to people with elevated resting heart rates. The heart is not pumping efficiently, while the pressure is increased in the blood.
Blood pressure will increase slightly during exercise to accommodate the need for a faster rate of blood flow.
 Try This
Try This
TR 1. Heart Rate Recovery

© David Kneafsey/iStockphoto
How long does it take your heart to return to its resting rate? First find your pulse at your wrist or under your jawbone. Record your pulse for 15 seconds and multiply by 4. This is your resting heart rate. Now, do jumping jacks or another vigorous activity for 1 minute. Immediately take your heart rate at the end of your exercise. Continue taking measurements every minute until your heart rate has returned to your resting rate. Plot these results on a graph of heart rate versus time.
If you have a physical condition that makes it inadvisable to exercise vigorously, try this alternative. After recording your resting heart rate, sit quietly, breathe deeply, and relax your body. After 4 minutes, check your heart rate to see how much you have lowered it. Take readings for every minute until your heart rate returns to its resting rate. Plot these results on a graph of heart rate versus time.
Go to your Lesson 2 Assignment to record your results.
1.14. Page 5
Module 8—Circulation, Immunity, and Excretion
 Read
Read
Cardiovascular Disorders and Treatments
© Sebastian Kaulitzki/shutterstock
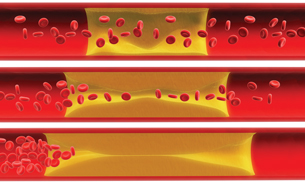
A common disorder of the circulatory system is a buildup of plaque (fat deposits) on the walls of the arteries. This disease, arteriolsclerosis, has many symptoms. The patient may feel chest pain, experience shortness of breath, and have high blood pressure. If the arteries continue to reduce in size, a blockage of an artery can lead to a stroke or a heart attack. Lifestyle choices such as smoking, a lack of exercise, and high-fat diets greatly increase the risk of developing this disease.
Look at the photo showing arteriolsclerosis. Imagine a garden hose. What happens to the flow of water when you put your thumb over the end of the hose to make the opening smaller? Water moves with greater force. By reducing the area that a fluid moves through, you will increase pressure. This is the same principle behind increased blood pressure due to arteriolsclerosis.
congenital: appearing at birth due to a heredity/genetic abnormality or from complications during a pregnancy
mitral stenosis: a heart valve disorder that narrows or obstructs the mitral valve opening
Some circulatory system problems are not a result of lifestyle choices. Many heart problems exist from birth and are congenital. Congenital heart defects include problems in the walls dividing the chambers of the heart and in the valves or in the structure of blood vessels around the heart. Many of these defects are detected at birth through a heart murmur, through blueness of the skin, or through technologies such as cardiac echocardiograms and cardiac catherizations. With the advancement of technology, many of these defects are being corrected with increasing success.
An example of a congenital heart disease is mitral stenosis. The mitral valve (which you know as the left bicuspid atrioventricular valve) is narrowed. It takes more effort for the left atrium to pump the blood through the narrowed valve to the left ventricle. This causes a rise in pressure in the left atrium. The walls of the left atrium then become thickened and the atrium enlarges.
Remember that flow moves from high pressure to low pressure. A back pressure of blood may then cause blood to move backwards in the blood vessels which bring blood to the left atrium (the pulmonary veins which bring blood from the lungs). This can be identified as an extra heart sound, or murmur, when a doctor uses a stethoscope. Also, the amount of blood leaving the ventricle is reduced. The heart does not pump efficiently and less blood reaches the body with each contraction, compared to a healthy heart. Some symptoms include fatigue, dizziness, or fainting.
Both arteriolsclerosis and mitral stenosis can be treated by surgery. Symptoms of the diseases can be controlled by medicine. Technological advances in medicine have been refined to help people regain homeostasis in their bodies.
Narrowing the mitral valve prevents the valve from opening properly and obstructs blood flow from the left atrium to the left ventricle. This can reduce the amount of blood that flows forward to the body.
Read “Cardiovascular Disorders and Treatments,” starting on page 277 of your textbook. You may want to make a chart of technologies that are used to diagnose and treat these disorders. This may help you when you come to your Unit D Assessment, where you will be conducting research. Save your chart in your course folder.
 Going Beyond
Going Beyond
Imagine that you are a surgeon who is performing a virtual heart transplant. Use the keywords “nova, virtual, and heart transplant” in a web search to locate the virtual activity.
Through this virtual operation you can see the steps involved in performing a transplant. It is amazing how far medical technology has progressed to benefit people.
 Module 8: Lesson 2 Assignment
Module 8: Lesson 2 Assignment
Remember to submit the Assignment answers to your teacher as part of your Module 8: Lesson 2 Assignment.
1.15. Page 6
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following essential questions:
- What is the relationship between the heart rate, blood pressure, and exercise?
- How can technology treat disorders of the circulatory system?
Average blood pressure and heart rates can be attributed to healthy lifestyles. This can include exercise and a balanced diet. Heart rate and blood pressure are a response to either a cardiovascular disorder or lifestyle choices. The heart rate increases as cellular respiration increases during vigorous exercise.
Exercise strengthens the heart muscle and can help prevent other cardiovascular diseases such as high blood pressure. Heart conditions and blockages in major blood vessels can be treated with advanced surgeries, while the symptoms can be managed with medicine. Diagnosing these diseases utilizes advanced imaging technology.
Lesson Glossary
arterial pressure: the pressure blood exerts on artery walls
congenital: appearing at birth due to a heredity/genetic abnormality or from complications during a pregnancy
diastole: the relaxation of the heart
mitral stenosis: a heart valve disorder that narrows or obstructs the mitral valve opening
Narrowing the mitral valve prevents the valve from opening properly and obstructs the blood flow from the left atrium to the left ventricle. This can reduce the amount of blood that flows forward to the body.
sphygmomanometer: a device used to measure blood pressure
stethoscope: an acoustic medical device designed to listen to internal sounds of the human body
systole: a contraction of the heart
1.16. Lesson 3 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 3—Blood
 Get Focused
Get Focused
So far, you have seen the comparison between the valves, pumps, and pipes of a water treatment plant and the circulatory system. Each of these systems works to move a specific fluid. A water treatment plant circulates water, while the circulatory system pumps blood.
As you discovered in previous lessons, water has many unique properties. One property is the ability to dissolve many chemicals, thus allowing the chemicals to be transported in biogeochemical cycles. What special properties of blood allow it to transport matter and energy for metabolic cycles?
In this lesson you will explore the following essential questions:
-
What are the main components of blood? How do these components contribute to transporting, clotting, and resisting the influence of pathogens?
-
How does blood help to regulate body temperature?
 Module 8: Lesson 3 Assignment
Module 8: Lesson 3 Assignment
Your teacher-marked Module 8: Lesson 3 Assignment requires you to submit a response to the following:
-
Lab: Identifying Blood Cells
-
TR 1. The Body’s Response to Temperature Change
You can access your Module 8: Lesson 3 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all the questions and place those answers in your course folder.
1.17. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Read
Read
connective tissue: the material between the cells of the body that gives tissues form and strength
This tissue is also involved in delivering nutrients.
undifferentiated cells: cells that have not yet reached the stage where specific biological roles are formed
These cells show no visible separation into their different structural parts
stem cells: undifferentiated cells that can theoretically divide without limit to replenish other cells
When a stem cell divides, each new cell has the potential to either remain a stem cell or become another type of cell with a more specialized function. This can be, for example, a muscle cell, a red blood cell, or a brain cell.
Blood is often referred to as a connective tissue. Its chief function is to connect blood cells with other tissues and body organs. It helps maintain homeostasis in a number of areas including water, nutrients, gas, hormones, and waste balance. Despite the fact blood appears to be uniform in its consistency, it is really made up of a solid, or formed, portion and a fluid portion.
The formed portion of the blood contains the cellular elements of
-
erythrocytes (red blood cells)
-
leucocytes (white blood cells)
-
platelets
These elements make up the formed portion of blood and are called this because these blood components are formed in the bone marrow from generic, undifferentiated cells—more commonly known as stem cells. These stem cells are capable of specializing and becoming any one of the three types of formed blood constituents.
© Sebastian Kaulitzki/iStockphoto
The following diagram illustrates the differentiation of blood cells.
microlitre: one millimetre cubed
hemoglobin: a protein that makes up the majority of the contents of a red blood cell
A human hemoglobin molecule contains four protein subunits attached to a heme group. One iron molecule, at the core of the heme group, binds one oxygen molecule. This ability to bind oxygen is essential in oxygen transport.
dissociates: to separate reversibly into smaller components
The fluid portion of the blood is the plasma that consists primarily of water (92%). The other 8% of the plasma contains
-
dissolved carbon dioxide
-
proteins (fibrinogen, albumin, globulin)
-
carbohydrates
-
phosphates
-
calcium, chlorine, potassium, and other minerals
-
vitamins
-
hormones
-
waste products like urea
1.18. Page 3
Module 8—Circulation, Immunity, and Excretion
 Read
Read
The Function of Blood
Transport: Red Blood Cells
© Sebastian Kaulitzki/shutterstock
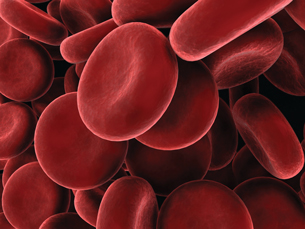
Red blood cells (erythrocytes) are the most plentiful cells in your blood. Women average 4.8 million RBCs/microlitre of blood. Men average 5.4 million RBCs/microlitre of blood. A microlitre is one-millionth of a litre. The number of blood cells can vary depending on health and altitude. At high altitudes, in order to cope with lower concentrations of oxygen, the body will increase red blood cell production.
Red blood cells are responsible for the transport of oxygen and carbon dioxide. The hemoglobin molecule makes it possible for RBCs to carry oxygen. When blood is pumped to the lungs, conditions in the blood cause hemoglobin to bind with oxygen. As the blood moves to capillaries in the lungs, there is a lower temperature, a higher pH, and an increase in oxygen pressure.
Oxygen, which has diffused through the alveoli, binds with the hemoglobin in the red blood cells. The hemoglobin is returned to the heart to be pumped to the rest of the body. As blood moves to capillaries in the rest of the body, there is a higher temperature, a lower pH, and lower oxygen pressure in the tissues. At this point, hemoglobin will give up its oxygen. Oxygen then diffuses into cells to be used as the final electron acceptor for cellular respiration.
Cellular respiration produces carbon dioxide. Most carbon dioxide is transferred into the RBC by diffusion, while some carbon dioxide remains in the plasma. Once inside the red blood cell, about half of the CO2 binds to sites on the hemoglobin molecule. The rest of the carbon dioxide will combine with water to form carbonic acid.
Carbonic acid dissociates into hydrogen ions(H+) and bicarbonate ions (HCO3-). Bicarbonate ions will diffuse back into the plasma. Hydrogen ions will bind to the hemoglobin molecule and therefore not increase the pH of the blood.
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3−
When red blood cells reach the lungs, the above reaction is reversed. Bicarbonate ions enter the red blood cells and combine with hydrogen ions to form carbonic acid. This is broken down into carbon dioxide and water. Carbon dioxide diffuses out of the red blood cells into the alveoli where carbon dioxide is released.
Anemia is a condition that occurs when there are too few red blood cells or too little hemoglobin inside red blood cells. Oxygen flow is reduced and a person will be tired and appear pale. Anemia can be caused by a lack of iron, which is a key component of hemoglobin. A diet that includes iron-rich foods such as red meat (in particular, liver), broccoli, and lentils can help alleviate anemia. You can also take iron supplements.
RBCs are terminally differentiated, which means they can never divide. They have a lifespan of about 120 days. Liver and spleen cells ingest blood cells at the end of their life cycles, and the iron from hemoglobin is reabsorbed into the body. The remaining portion of the blood cells are degraded into bile pigments, which are secreted by the liver. The liver scavenges approximately three million RBCs per second.
1.19. Page 4
Module 8—Circulation, Immunity, and Excretion
Clotting: Platelets
shock: a serious, life-threatening condition where insufficient blood flow reaches the body tissues
As the blood carries nutrients and oxygen around the body, reduced flow hinders the delivery of these components to the tissues, and can stop the tissues from functioning properly.
coagulation: the process where a damaged blood vessel wall is covered by a platelet and fibrin- containing clot to stop bleeding and begin repair of the damaged vessel
fibrin: a mesh-like protein involved in the clotting of blood
Platelets are cell fragments of larger cells called megakaryocytes. You normally have about 150 000 to 400 000 platelets/µl of blood. The number of platelets in your bloodstream is controlled by a negative feedback system. If there are too many platelets, their production is inhibited. If there are not enough platelets in the blood, their production will be stimulated. If this value should drop much below 50,000/µl, there is a danger of uncontrolled bleeding because of the essential role that platelets have in blood clotting.
When blood vessels are cut or damaged, the loss of blood from the system must be stopped before shock and possible death occur. This is accomplished by solidification of the blood, a process called clotting or coagulation. The process of coagulation has many steps. You may read about these steps on pages 283 and 284 of the textbook.
A blood clot consists of a plug of platelets enmeshed in a network of insoluble fibrin molecules. The blood clot stimulates the growth of the structural framework and smooth muscle cells within the vessel wall. The repair process begins, and the blood clot is dissolved.
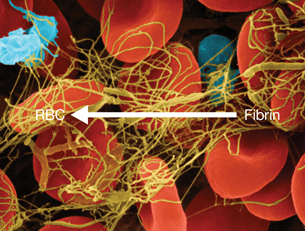
Copyright Dennis Kunkel Microscopy, Inc.
Hemophilia is a disease where the body does not have the ability to stimulate the production of a mesh–like network of fibrin molecules. As a result, an injured blood vessel in a hemophiliac will continue to lose blood for a longer period of time, and no blood clot will form. Healing also takes a longer time, which often increases the likelihood of infection or a reopening of the wound. Hemophiliacs can receive injections of a chemical that will stimulate the production of fibrin.
1.20. Page 5
Module 8—Circulation, Immunity, and Excretion
Response to Invading Pathogens: White Blood Cells
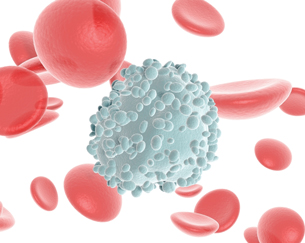
© sgame /shutterstock
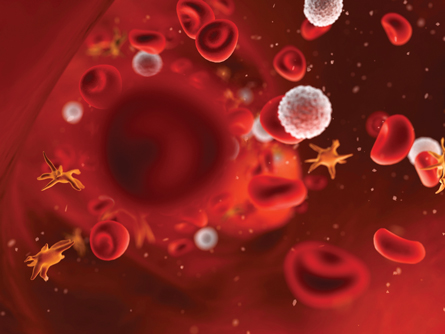
White blood cells are less numerous than red blood cells by a ratio of 1:700. White blood cells contain a nucleus and are able to divide, unlike red blood cells. The ultimate role of white blood cells is to participate in protecting the body from infection.
As outlined in the “Differentiation of Blood Cells” diagram at the beginning of the lesson, white blood cells consist of lymphocytes and monocytes with relatively clear cytoplasm. These cells have three types of granulocytes, whose cytoplasm is filled with granules.
Lymphocytes are B-cells and T-cells. B-cells are responsible for making antibodies. T-cells assist B-cells in making antibodies, kill invading viruses or other pathogens by phagocytosis, regulate B-cell response, or remember returning pathogens.
antibody: a protein in the blood that identifies and neutralizes foreign invaders, such as bacteria or viruses
Each antibody is specific to a particular invader.
pathogen: a germ or foreign-invading substance that can cause illness/disease
Monocytes leave the blood and become macrophages. Macrophages are large, phagocytotic cells that engulf and destroy foreign material that enter the body, or they destroy dead or dying body cells.
Granulocytes consist of three different cell types—the neutrophils, the eosinophils, and the basophils.
Neutrophils are the most abundant of the white blood cells. Neutrophils squeeze through the capillary walls and into infected tissue where they kill the invaders, such as bacteria, and then engulf the remnants. This is a never-ending task, even in healthy people—throats, nasal passages, and colons contain vast numbers of bacteria.
Most of these bacteria do people no harm because neutrophils keep the bacteria in check. However, heavy doses of radiation, chemotherapy, and many other forms of stress can reduce the numbers of neutrophils so that formerly harmless bacteria begin to proliferate. The resulting opportunistic infection can be life-threatening.
Eosinophils store many toxins in the granules within the cell. These cells circulate in the blood and migrate to inflamed sites or specific areas of parasitic worm infection. Unless there is an infection or a parasitic worm, the levels of eosinophils in the blood are very low (0-450/µl). When they are needed, the eosinophil releases toxic granules that will kill the invading parasite or pathogen.
Basophils are also in relatively low concentrations unless the body is fighting an infection. Basophils leave the bloodstream and accumulate at the site of an inflammation or infection. The contents of granules are released, which, instead of killing invaders, increase blood flow to an area. Increased basophil concentrations are evident during an allergic reaction.
1.21. Lab
Module 8—Circulation, Immunity, and Excretion
 Lab: Identifying Blood Cells
Lab: Identifying Blood Cells
You will now perform a modified version of “Investigation 8.C: Identifying Blood Cells” from page 285 in the textbook. Note: You will not be using the light microscope as described in the textbook lab, but rather a set of ten prepared online slides.
You will be assuming the role of a lab technician in this virtual investigation. Virtual slides with smears of different blood samples will be presented to you so you can identify what kinds of cells are present.
Background Information
Have you ever had a blood test? It is common that a complete blood count, or CBC, is ordered as part of the test. The CBC measures the number of red blood cells, the number of white blood cells, the total amount of hemoglobin in red blood cells, and the fraction of the blood composed of red blood cells (the hematocrit). The hematocrit part of the CBC test measures the number and size of red blood cells. It gives a measure of the proportion of the whole blood that is made up of red blood cells. The value is then given as a percentage, such as 45%, which means that red blood cells take up 45% of the blood volume.
How the Test Is Performed
Blood is usually drawn from the inside of the elbow or the back of the hand. The site is cleaned with antiseptic and an elastic band is placed around the upper arm to apply pressure and restrict blood flow through the vein. This causes veins below the band to swell with blood.
A needle is inserted into the vein, and the blood is collected in an air-tight vial or a syringe. During the procedure, the band is removed to restore circulation. Once the blood has been collected, the needle is removed, and the puncture site is covered to stop any bleeding.
In the laboratory, some of the blood is centrifuged (spun in a machine). This forces the cells to the bottom of the container. The cellular portion is compared with the total amount of blood and expressed as a percent. The cellular portion is composed almost entirely of red blood cells. The percentage of white blood cells is very small.
What Abnormal Results May Mean
Low hematocrit may indicate
- anemia
- blood loss (hemorrhage)
- bone marrow failure (affects stem cell production) (e.g., due to radiation, toxin, fibrosis, tumour)
- destruction of red blood cells
- leukemia
- malnutrition or specific nutritional deficiency
- multiple myolema (cancer of plasma cells in the bone marrow)
- rheumatoid arthritis
High hematocrit may indicate
- dehydration
- burns
- diarrhea
- erythrocytosis (excessive red blood cell production)
Procedure
In order to more easily identify the blood cells found in the histology slides, click on the following link and read about the characteristics of a blood smear.
If you need more help distinguishing between white and red blood cells, look at the following link.
Work through the four different suggestions to differentiate the leukocyte cell types.
Suggestions:
- Are cytoplasmic granules present or absent?
- Determine the colour of the granules (red or blue).
You can read about this in the following link.
- What does the nucleus look like?
You can read about this in the following link.
- Use RBCs as a size comparison.
You can read about this in the following link.
Once you are confident that you are able to differentiate between the cells, continue with the investigation.
Perform the Differential Counts activity, and view the ten fields or slides.
Now continue with the Lab in the Assignment.
 Read
Read
Transport: Plasma
Plasma carries all of the blood cells as well as transporting wastes, nutrients, and hormones. Without the bloodstream to serve as a pathway for hormones, the body is unable to respond effectively to fluctuations in its external or internal environment. Many regulatory feedback systems are dependent on the presence of hormones. If feedback systems are out of balance, many different parts of the body will cease to function together. If so, your body will break down.
You may want to read more on the role of plasma in the transport of matter on pages 284 and 285 of the textbook.
 Self-Check
Self-Check
SC 1. Complete this Self-Check activity about blood.
Now continue with the Lab in the Assignment.
1.22. Page 7
Module 8—Circulation, Immunity, and Excretion
 Read
Read
Homeostatic Regulation
countercurrent heat exchange: a mechanism used to transfer heat from one flowing current of fluid to another across a semi-permeable membrane
Birds use countercurrent heat exchange between blood vessels in their legs to keep heat concentrated within their bodies.
vasoconstriction: the constriction of blood vessels resulting from muscular contraction in blood vessel walls
When blood vessels constrict, the flow of blood is restricted or slowed. It is the opposite of vasodilation, the widening of blood vessels.
Blood also plays a role in maintaining body temperature. Maintaining body temperature means that your body is balancing heat production with heat loss. This is achieved by a countercurrent heat exchange mechanism. On average, the recognized human core body temperature is 37°C. In the face of extreme exertion, cellular respiration within muscles generates a significantly higher amount of heat than resting muscle tissue. It can be 10 to 20 times more in some circumstances.
How does your body cope? Because plasma is mostly water, it has the capacity to absorb and release large amounts of thermal energy. (Remember specific heat capacity from Science 10.)
 Watch and Listen
Watch and Listen
This animation illustrates peripheral heat loss, countercurrent heat exchange, and selective vasoconstriction. You may want to first read “Homeostatic Regulation” on pages 286 and 287 of the textbook.
 Self-Check
Self-Check
SC 2. How does blood link the circulatory system with other systems?
SC 3. Name three factors that can trigger vasoconstriction or vasodilation.
 Self-Check Answers
Self-Check Answers
SC 2. Blood links the circulatory system with other systems by a network of blood vessels. These vessels allow substances to move in and out of the bloodstream to be transported to other parts of the body or to the external environment.
SC 3. Factors that can trigger vasoconstriction are high blood pressure, drugs, and cold weather. Factors that can trigger vasodialation are physical exertion, low blood pressure, and drugs/chemicals such as caffeine.
 Try This
Try This
TR 1. The Body’s Response to Temperature Change
Thermoregulation is the term used when biological systems attempt to maintain temperature. After watching the previous animations and reading the textbook, prepare a summary table. Outline the body’s thermoregulatory response to
- an increase in internal temperature due to exertion
- a colder external temperature than body temperature
Explain how peripheral heat loss, selective vasoconstriction, vasodilation, and countercurrent heat exchange are involved in each circumstance.
Record your responses/summary table in the Lesson 3 Assignment.
1.23. Page 8
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect
Reflect and Connect
 Self-Check
Self-Check
SC 4. All of the following are functions of blood except
- defense against infection
- transportation of oxygen
- synthesis of vitamins
- regulation of body temperature
SC 5. What are the formed elements of blood?
- erythrocytes, leukocytes, and platelets
- blood cells and plasma proteins
- blood cells, cell fragments, and plasma
- blood cells and cell fragments
SC 6. All of the following are true of erythrocytes except
- their plasma membrane contains many surface antigens
- they transport oxygen from the lungs to body tissues
- they have a finite life span averaging only about 60 days
- when mature, they have no nucleus or other organelles
SC 7. Which formed elements help initiate an immune response and defend the body against pathogens?
- erythrocytes
- leukocytes
- platelets
- all of the above
SC 8. Monocytes are agranulocytes that leave the circulation after a few days to become
- lymphocytes
- macrophages
- microphages
- megakaryocytes
 Self-Check Answers
Self-Check Answers
SC 4. C
SC 5. A
SC 6. C
SC 7. B
SC 8. B
 Module 8: Lesson 3 Assignment
Module 8: Lesson 3 Assignment
Remember to submit the Assignment answers to your teacher as part of your Module 8: Lesson 3 Assignment.
1.24. Page 9
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following essential questions:
-
What are the main components of blood? How do these components contribute to transporting, clotting, and resisting the influence of pathogens?
-
How does blood help to regulate body temperature?
Blood is a multifaceted component of your circulatory system. Specialized cells in blood each serve a function.
Red blood cells carry oxygen and carbon dioxide. There are five kinds of white blood cells.
Lymphocytes produce antibodies and regulate the production of antibodies. Eosiniophils release toxic granules, which kill pathogens. Neutrophils are macrophages that engulf and destroy invading pathogens, while basophils release granules that will increase blood flow to an area of infection, thus increasing inflammation.
Monocytes are also macrophages and engulf and destroy invading pathogens. Platelets are the cellular component in blood that ensure blood clotting occurs in the event of a ruptured blood vessel. Plasma, the fluid portion of blood, is key in transporting nutrients, hormones, and exchanging heat. Since plasma is mostly water, the heat capacity of water allows plasma to absorb and release large amounts of energy created during cellular respiration.
Your body is designed to balance heat production with heat loss via a countercurrent heat exchange mechanism. The close proximity of blood vessels allows transfer of thermal energy from warmer areas to cooler areas. This heat exchange system allows your body to adapt to varying internal and external conditions.
Finally, the movement of blood through the capillaries is essential to the transport of matter. Because of concentration and pressure gradients, the movement of wastes, essential nutrients, and fluids is possible. A disruption to these gradients can cause dysfunction in the body.
Lesson Glossary
antibody: a protein in the blood that identifies and neutralizes foreign invaders, such as bacteria or viruses
Each antibody is specific to a particular invader.
coagulation: the process where a damaged blood vessel wall is covered by a platelet and
fibrin-containing clot to stop bleeding and begin repair of the damaged vessel
connective tissue: the material between the cells of the body that gives tissues form and strength
This tissue is also involved in delivering nutrients.
countercurrent heat exchange: a mechanism used to transfer heat from one flowing current of fluid to another across a semi-permeable membrane
Birds use countercurrent heat exchange between blood vessels in their legs to keep heat concentrated within their bodies.
fibrin: a mesh-like protein involved in the clotting of blood
pathogen: a germ or foreign-invading substance that can cause illness/disease
shock: a serious, life-threatening condition where insufficient blood flow reaches the body tissues
As the blood carries nutrients and oxygen around the body, reduced flow hinders the delivery of these components to the tissues, and can stop the tissues from functioning properly.
stem cells: undifferentiated cells that can theoretically divide without limit to replenish other cells
When a stem cell divides, each new cell has the potential to either remain a stem cell or become another type of cell with a more specialized function. This can be, for example, a muscle cell, a red blood cell, or a brain cell.
undifferentiated cells: cells that have not yet reached the stage where specific biological roles are formed
These cells show no visible separation into their different structural parts.
vasoconstriction: the constriction of blood vessels resulting from muscular contraction in blood vessel walls
When blood vessels constrict, the flow of blood is restricted or slowed. It is the opposite of vasodilation, the widening of blood vessels.
1.25. Lesson 4 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 4—Circulation

© Peter Wey/shutterstock
 Get Focused
Get Focused
In a water treatment plant, pipes become smaller as you work through the filtration process. In the circulatory system, the smallest pipes are capillaries. Fluids move through blood vessels (as with any kind of pipe) when there is a pressure difference between the start and end of the pipe.
Just as water moves continuously as a river flows downhill, the pressure drops continuously from the start to the end of a vessel. How does this affect the transportation of nutrients to all cells of the body?

© Andrea Danti/shutterstock
© Robert Adrian Hillman/shutterstock
In this lesson you will explore the following essential question:
- At the capillary level, how does the circulatory system aid the digestive, excretory, respiratory, and motor systems’ exchange of matter with the environment?
 Module 8: Lesson 4 Assignment
Module 8: Lesson 4 Assignment
Your teacher-marked Module 8: Lesson 4 Assignment requires you to submit a response to the following:
- TR 1. Capillary Fluid Exchange
You can access your Module 8: Lesson 4 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all the questions and place those answers in your course folder.
1.26. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
Circulation and the Action of Capilliaries
Capilliaries are the smallest blood vessels in the body. They are the only vessels thin enough for the exchange of matter by diffusion. The cells of the body are constantly bathed in interstitial fluid, or extracellular fluid. Any material exchanged must pass through the interstitial fluid. The exchange of matter from capillary to interstitial fluid or vice versa is dependent on concentration gradients.
Substances move from high concentrations to low concentrations. This is referred to as a concentration gradient. Blood flow is also dependent on pressure differences. Fluid moves from high pressure to low pressure. Therefore, the pressure in the capillaries is lower than it is in the arteries, but higher than in the veins. This ensures unidirectional blood flow.
hydrostatic pressure: the pressure exerted by a fluid on any contacting surface, such as the force exerted by blood on a capillary wall
Hydrostatic pressure is greater on the arteriole end of a capillary.
osmotic pressure: hydrostatic pressure produced by a solution that is separated by a semi-permeable membrane
The pressure is created due to different concentrations of solutes. It is required to maintain equilibrium with no net movement of solvent. In other words, osmotic pressure stays the same at all times unless there is a problem. You can think of osmotic pressure as the pressure required to prevent water from leaving.
Plasma Interstitial Fluid Exchange
The aqueous solutions that compose the plasma and the interstitial fluid readily exchange through the thin walls of most of your body's capillaries. The forces that govern this exchange are hydrostatic pressure (the blood pressure within the capillaries) and osmotic pressure.
Hydrostatic Pressure
The capillary wall acts as a filtration barrier. Most of the fluid within the capillaries is retained, but some fluid filters through pores between the cells. This fluid is pushed by the pressure difference between the capillary blood and the interstitial fluid. Water and small solutes can pass freely through these pores.
Hydrostatic pressure is based on the loss of water and solutes from the capilliary. At the arteriol end of a capillary, the hydrostatic pressure is higher because not much water or solutes (nutrients) have diffused out of the capillary. At the venous end of the capillary, the hydrostatic pressure is lower because substances have diffused out of the capillary and into the interstitial fluid and other cells. The capillary walls (both cells and pores) are impermeable to the plasma proteins and lipids. Under normal pressure conditions, the proteins and lipids stay within the plasma. However, if there is an imbalance, proteins and lipids may leave the plasma.
With hydrostatic pressure, water is more highly concentrated in the capillary. This influx of water from osmosis increases the hydrostatic pressure in the capillary. This tends to force the water back to the interstitial fluid. Hydrostatic pressure will be greater at the arteriol end. This means there will be more water in the capillary in relation to other solutes. As solutes and water leave the blood, the hydrostatic pressure decreases toward the venous end of the capillary.

Osmotic Pressure
Because the capillary wall is permeable to water, but essentially impermeable to plasma proteins, these molecules generate an osmotic pressure. This results in a pressure that draws water from the interstitial fluid into the blood plasma. Osmotic pressure remains constant over the length of a capillary.

In the diagram to the left, the force exerted by water inside the capillary will eventually equal the force of diffusion from the interstitial fluid, creating equilibrium. When equilibrium is reached, water continues to flow, but it flows both ways in equal amounts as well as forces. This is why osmotic pressure remains constant over the length of a capillary.
Hydrostatic pressure tends to cause fluid to leave the plasma, and osmotic pressure pulls it back. These two forces balance each other under normal conditions.
Hydrostatic pressure gradually decreases over the length of a capillary, while osmotic pressure remains constant. If these pressures were graphed, they would look approximately like the following figure.
1.27. Page 3
Module 8—Circulation, Immunity, and Excretion
 Watch and Listen
Watch and Listen
Fluid Exchange Across the Walls of Capillaries
You may want to read “Circulation and the Action of Capillaries” on pages 287 and 288 of the textbook and study “Figure 8.22” before you watch this animation.
 Self-Check
Self-Check
SC 1. How would serious bleeding affect the movement of fluids in and out of the capilliary?
SC 2. Why does blood not flow constantly through the billion capillaries in your body?
SC 3. Where does the diffusion of materials take place in a capillary?
SC 4. Why is blood flow slower through capillaries?
SC 5. What determines the direction of diffusion?
SC 6. Based on what you know about the movement of fluids and materials, hypothesize why a child who has a lack of nutritious food will have a distended abdomen.
 Self-Check Answers
Self-Check Answers
SC 1. Bleeding would reduce the pressure and concentration gradients. Therefore, the diffusion of essential nutrients and gases would be inhibited. Cells would not exchange materials and then cease to function properly, leading to shock.
SC 2. Blood does not constantly flow to all capillaries because cells may not need to be serviced or blood may be needed elsewhere. For example, capillaries of the digestive system are open after you have eaten, but they are closed to certain muscle cells.
SC 3. The diffusion of materials takes place along the mid-section of a capillary.
SC 4. Blood flow is slower through capillaries to allow diffusion to take place.
SC 5. The direction of diffusion is determined by concentration and pressure gradients.
SC 6. A child lacking proper nutrition will have a distended abdomen because fluid has moved from high concentrations to low concentrations. Because there are no/few nutrients in the blood plasma of the capilliaries in the digestive system, the relative concentration of fluid is high. Fluid will leave the blood, causing tissues to swell.
 Try This
Try This
TR 1. Capillary Fluid Exchange
You will now apply your knowledge of the capillary fluid exchange model to three new circumstances. In each situation the hydrostatic pressure or the osmotic pressure have changed from their normal levels. Decide what the net movement of the water will be, either outward or inward. Create a diagram or sketched summary of each situation.
Your illustration should start at the capillary level, with the hydrostatic pressures, osmotic pressures, and net movement of water represented by arrows. Each situation will present you with one question. Be sure to answer each question by describing the physiological changes that would occur in an individual with each of the three conditions as a result of this net movement of water.
Go to your Module 8: Lesson 4 Assignment to complete this activity.
1.28. Page 4
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect
Reflect and Connect
 Try This
Try This
TR 2. Capillary Action in Different Systems
Describe what is happening, in terms of exchange of matter, in each of the following systems:
- motor
- respiratory
- digestive (excluding the example of the large intestine)
- excretory
Explain how the concentration gradient and pressures would move matter specific to each system in and out of the circulatory system.
For example, capillaries in the large intestine would absorb water and deposit nutrients. The amount of water in cells and interstitial space surrounding large intestine cells would be high in comparison to the capillary, since the job of the large intestine is to absorb water.
The difference between hydrostatic pressure and osmotic pressure would cause water to enter the capillary to be distributed to other parts of the body requiring water. Nutrients and oxygen would diffuse out of the capillary. The pressure difference from the arteriole to the venous end of the capillary ensures that blood flows in one direction.
Record your responses in your course folder as a review of the role of the capillaries in matter exchange.
 Module 8: Lesson 4 Assignment
Module 8: Lesson 4 Assignment
Remember to submit the Assignment answers to your teacher as part of your Module 8: Lesson 4 Assignment.
1.29. Page 5
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following essential question:
- At the capillary level, how does the circulatory system aid the digestive, excretory, respiratory, and motor systems’ exchange of matter with the environment?
Matter exchange between the circulatory system and all other body systems occurs because of fluid pressure in the interstitial fluid and the capillary. The pressures determine relative concentration gradients of other molecules that must diffuse in and out of the capillaries. Substances will move from high concentrations to low concentrations. These concentrations are mediated by the difference between osmotic pressure and hydrostatic pressure.
As blood moves from the arteriole to the venous end of a capillary, pressures will change. The pressure is maintained because fluid leaving the capillary equals the fluid entering the capillary. Because of concentration gradients, substances such as oxygen will diffuse out of the capillary while carbon dioxide will diffuse into the capillary.
Lesson Glossary
hydrostatic pressure: the pressure exerted by a fluid on any contacting surface, such as the force exerted by blood on a capillary wall
Hydrostatic pressure is greater on the arteriole end of a capillary.
osmotic pressure: hydrostatic pressure produced by a solution that is separated by a semi-permeable membrane
The pressure is created due to different concentrations of solutes. It is required to maintain equilibrium with no net movement of solvent. In other words, osmotic pressure stays the same at all times unless there is a problem. You can think of osmotic pressure as the pressure required to prevent water from leaving.
1.30. Lesson 5 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 5—The Lymphatic System and Immunity
 Get Focused
Get Focused

© mike.irwin/shutterstock
Water treatment plants in most of North America have a process that eliminates harmful waterborne bacteria and parasites that may be present in natural water. Ultraviolet light is used to kill organisms in the water.
Chemicals such as chlorine are also added to the water to kill micro-organisms, but the levels are not harmful to the overall health of humans. Your lymphatic and immune systems also use processes to remove harmful substances to prevent you from being ill. Only harmful invaders or dead cells are recognized and destroyed by your body. Water treatment plants have human operators and computers to determine water quality and intensity of treatment. How does the human body determine its response to invading substances?
In this lesson you will explore the following essential questions:
- What is the function of the lymphatic system?
- How do the cellular and non-cellular components of the human defense system work together to maintain homeostasis?
 Module 8: Lesson 5 Assignment
Module 8: Lesson 5 Assignment
Your teacher-marked Module 8: Lesson 5 Assignment requires you to submit a response to the following:
- TR 1. An Immune Response
- Reflect and Connect: A Creative Representation of the Immune System
You can access your Module 8: Lesson 5 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all the questions and place those answers in your course folder.
1.31. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Watch and Listen
Watch and Listen
The following video “The Immune System: Your Magic Doctor” describes the function of the immune system by
- listing the major parts of the system
- describing the mechanical barriers to infection
- primary response by macrophages
- action of antibodies
- differences between viral and bacterial infections
- role of suppressor T-cells and memory cells after an infection has been cleared up
Allergic reactions, autoimmune diseases, mutations, cancer, immunodeficiency, and vaccination also are described.
 Self-Check
Self-Check
SC 1. What is your body’s first line of defence?
SC 2. What does the body refer to as “your magic doctor”?
SC 3. Where are B-cells and T-cells stored?
SC 4. What do macrophages do?
SC 5. What can damage macrophages?
SC 6. What do helper T-cells do?
SC 7. What do B-cells do?
SC 8. What do antibodies do?
SC 9. Why are viruses a “sneaky” invader and hard to get rid of?
SC 10. What do killer, suppressor, and memory T-cells do?
SC 11. What is an allergic reaction?
SC 12. What is it called when the immune system attacks healthy cells?
SC 13. Give an example where the immune system may fail.
SC 14. How does HIV interfere with the immune system?
SC 15. How does immunization work?
SC 16. What are symptoms of infection?
SC 17. Why does exercise help the immune system?
 Self-Check Answers
Self-Check Answers
SC 1. The body’s first line of defence is the skin, coughing, sneezing, vomiting, cilia/hairs that trap particles, eyelashes, eyelids, mucus in the nose and mouth, and tears.
SC 2. Your magic doctor is your immune system.
SC 3. B-cells are stored in lymph nodes, while T-cells are stored in glands near the heart called thymus glands.
SC 4. Macrophages engulf and digest invading bacteria.
SC 5. Macrophages can be damaged by invading pathogens or smoking.
SC 6. Helper T-cells identify antigens on invading pathogens and send messages to B-cells.
SC 7. B-cells begin producing antibodies specific to the invading antigen.
SC 8. Antibodies attach themselves to the antigens of the invaders. This marks and/or neutralizes the invader and the invader is unable to resist attack by macrophages and other white blood cells.
SC 9. Viruses take over regular cells and are able to multiply and destroy the regular cells in the process.
SC 10. Killer T-cells kill host cells containing viruses and the virus itself. Suppressor T-cells make sure that once the viruses are killed, the killer T-cells don’t harm healthy cells. Memory T-cells remember the type of invader antigens so that the immune system can respond faster.
SC 11. An allergic reaction is when the body views a harmless substance like food or pollen as a foreign invader and attacks the pathogen. An allergic reaction may cause symptoms like swelling, sneezing, or itching.
SC 12. When the immune system attacks healthy cells, it is called an autoimmune disease.
SC 13. The immune system may fail to recognize some viruses or cancer cells.
SC 14. HIV interferes with the immune system by killing helper T-cells.
SC 15. A similar virus is injected into the body. Antibodies are produced to kill this virus and memory T-cells remember the antigen, so an immune response can happen when a virus invades the body again.
SC 16. Symptoms of infection are redness, swelling, pus, swollen lymph nodes, fever, and pain.
SC 17. Exercise helps the body to use nutrients properly and reduces stress.
The Lymphatic System
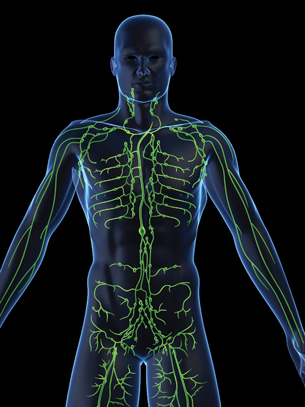
© Sebastian Kaulitzki/shutterstock
If asked to comment on the circulatory system, you could probably, without difficulty, describe its anatomy and list a number of roles that the circulatory system performs. When asked a similar question about the structure and function of the lymphatic circulatory system (or simply the lymphatic system), you may be less familiar with the anatomy. The lymphatic circulatory system is a network of vessels with associated glands or nodes that extends throughout the body.
You might not think about the lymphatic system until you are sick. Swollen lymph nodes under the jaw or armpits can be painful and cause concern. This system plays a critical role in the maintenance of the body’s fluid and osmotic balance. The lymphatic system is much like the venous portion of the circulatory system. It is a network of one-way vessels that collects the fluid that “leaks” from the capillaries into the interstitial (or extracellular) space between cells.
You may access an animation describing the lymph nodes by doing a web search. Use the keywords “how stuff works lymph nodes.”
 Read
Read
Continue learning about the lymphatic system by reading pages 292 and 293 of the textbook. Pay close attention to the diagrams to see the relationship between the circulatory system and the lymphatic system.
 Self-Check
Self-Check
SC 18. How is the lymphatic system related to the circulatory system?
SC 19. How does the lymphatic system help to protect the body from infection?
 Self-Check Answers
Self-Check Answers
SC 18. Lymph vessels are closely associated with the capillaries of the cardiovascular system. Fluid that escapes from the cardiovascular capillaries forms part of the interstitial fluid. Some of this fluid is collected in the lymphatic capillaries and is eventually returned to the blood.
SC 19. The lymphatic system also works with the white blood cells to protect the body against infection. White blood cells called lymphocytes mature in the lymph nodes, which are the glands found throughout the lymphatic system. The lymph nodes also contain macrophages, which trap and destroy bacteria that are circulating within the body.
1.32. Page 3
Module 8—Circulation, Immunity, and Excretion

© Anna Dzondzua/shutterstock
The Defence System
Your body is constantly under siege by a variety of micro-organisms. These organisms are looking to enter and establish a home in which to live and reproduce. Many of these foreign invaders are harmless. However, a large number of these bacteria, protozoa, fungi, and viruses are pathogenic—or dangerous—and may even be deadly to the body.
The human body uses a number of protective mechanisms to defend itself from these potentially hostile pathogens. The first line of defence is to deny the micro-organisms entry into the body.

© carlo dapino/shutterstock
The skin is a continuous barrier that prevents access. The epithelial (surface) cells of the skin protect against the billions of organisms you are exposed to on a regular basis. There is additional support at potential weak spots in people’s external covering. For example, tears and eyelashes protect the eyes, cilia and mucus protect the respiratory tract, and stomach acid protects the digestive system. Together, these defences repel the vast majority of pathogens.
As effective as the physical and chemical barriers of the body are, there may occasionally be a breach in the defence system. When pathogens are provided access to people’s internal systems by breaches such as cuts or scrapes, the second line of defence is called into action. Macrophages and other phagocytotic cells surround and engulf the invading pathogens. This is a non-specific defence, or cell-mediated immunity, which include neutrophils, monocytes, and T-cells.
The T-cells involved in the cell-mediated (non-specific) immune response are specialized to perform a number of functions. Helper, killer, suppressor, and memory T-cells all play specific roles. They not only defeat pathogens but also ensure that the body is protected from further infections. By ridding the body of pathogens, the lymphatic system and immunity maintain homeostasis.
cell-mediated immunity: involves the activation of white blood cells, specifically macrophages, neutrophils, monocytes, and T-cells rather than the production of antibodies
helper T-cell: arises from the thymus
These T-cells recognize an antigen on the surface of an invading pathogen and stimulate B-cells to produce antibodies.
killer T-cell: also known as a cytotoxic T-cell
It kills other target cells, such as cells infected with viruses, parasites, or cancer. These T-cells monitor all the cells of the body and are ready to destroy any cells that express foreign antigen fragments on the surface.
suppressor T-cell: slows and suppresses the process of cellular immunity to ensure that normal tissue does not get destroyed
memory T-cell: a lymphocyte that carries receptors for a specific foreign antigen encountered in an earlier infection or through vaccination; it quickly promotes an immune response if the same antigen is re-encountered in a subsequent infection
 Watch and Listen
Watch and Listen
Watching the following four animations may help you visualize how immunity works. You do not need to watch all of the animations:
- The following animation, “Battles in the Bloodstream,” shows how white blood cells work together to initiate an immune response to an invading pathogen.
- Click on “Cytotoxic T-Cell Activity Against Target Cells” to see how killer T-cells come to identify viruses that have invaded regular cells.
- “Constructing Vaccines” illustrates how injecting inactivated or weakened strains of a particular pathogen stimulates the body to create antibodies.
- “IgE Mediated (Type 1) Hypersensitivity” shows, at the cellular level, how people become allergic to or are affected by certain pathogens. IgE stands for immunoglobulin E, which is an antibody that plays an important role in allergic reactions. Immunoglobulin is just another word for antibody. The animation makes reference to mast cells. You have been previously introduced to mast cells as basophils or eosinophils.
The Third Line of Defence
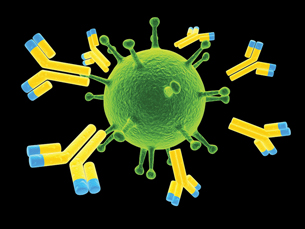
© Sebastian Kaulitzki /shutterstock
The third line of defence is antibody-mediated immunity. Antibodies in the bloodstream will recognize foreign substances and act to neutralize or destroy them.
Antibodies are “Y” shaped molecules. The amino acid sequence in the tips of the "Y" varies greatly among different antibodies. This variation of amino acids makes the antibody specific for particular antigens. Think of an antibody as a cellphone number and an antigen as the person you are calling. The 10-digit cell number is specific to the person you are calling. An antibody is specific to an antigen.
Antibodies contribute to immunity in three main ways: They can prevent pathogens from entering or damaging cells by binding to antigens; they can stimulate the removal of a pathogen by macrophages and other cells by coating the pathogen; and they can trigger direct pathogen destruction by stimulating other immune responses.
For example, antibodies will bind to surface antigens on an invading bacterium. This can prevent the bacteria from entering and damaging healthy cells. The antibodies can also attract macrophages to engulf and destroy the bacterium. Thirdly, the antibody may stimulate a response where granulocytes (basophils, eosinophils, or neutrophils) will release their toxic granules and killer T-cells will release toxic molecules that ultimately results in the destruction of the invading bacteria.
Symptoms of this kind of reaction include swelling, fever, pus, or redness and indicate infection. Symptoms of infections, however, indicate that the immune system is working to regain homeostasis.
 Read
Read
You may want to continue to read pages 293 to 295 of the textbook before you attempt the following activities. “Figure 8.27” on page 294 provides a clear illustration of your body’s immune response.
 Try This
Try This
TR 1. An Immune Response
Your body exhibits two types of immune response. Go to your Lesson 5 Assignment to complete an activity that explores immune responses.
1.33. Page 4
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect: A Creative Representation of the Immune System
Reflect and Connect: A Creative Representation of the Immune System
Scientists often create simulations or models to illustrate how something works. Models and simulations are useful tools in visualizing biological processes. A model is a logical representation of a phenomena or process. The following graphic is an example of such a model.
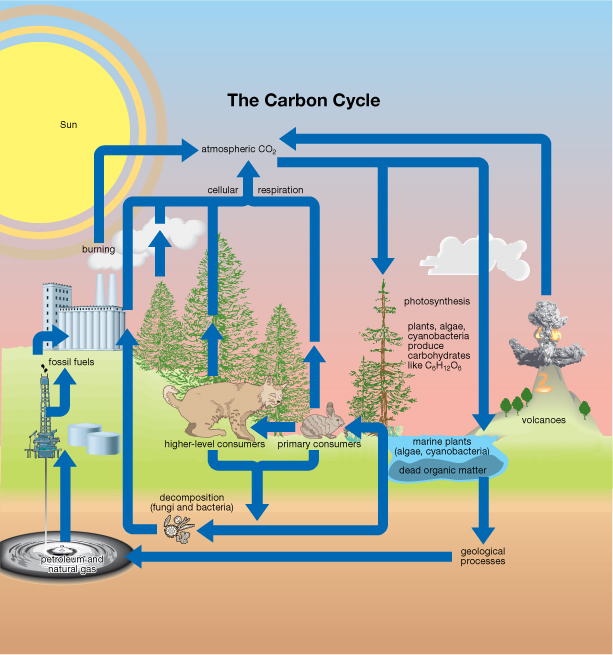
Any of the animations you have viewed in this course can be used as an example of a simulation.
Based on your current knowledge and further research of the lymphatic system and immunity, you will design a model or simulation of the functioning of the main components of the human immune system. You will model the body’s immune response from the first line of defence to the third line of defence and identify all cells and components involved in an immune response.
Your presentation may be in any format suitable such as illustrations, animations, video, or a slide show.
Go to your Lesson 5 Assignment for further instructions.
 Reflect on the Big Picture
Reflect on the Big Picture
 Discuss
Discuss

© VectorZilla/shutterstock
A minority of individuals may have allergies to peanuts or other foods. Should students be restricted from bringing these food items into the school lunchroom? Post your argument in the discussion area. What do other students have to say?
 Going Beyond
Going Beyond
What is the relationship between immunity and breast feeding? Conduct web research to see what you can find out. Record your findings in your course folder.
 Module 8: Lesson 5 Assignment
Module 8: Lesson 5 Assignment
Remember to submit the Assignment answers to your teacher as part of your Module 8: Lesson 5 Assignment.
1.34. Page 5
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following essential questions:
- What is the function of the lymphatic system?
- How do the cellular and non-cellular components of the human defence system work together to maintain homeostasis?
The constant battle waged within your body to turn back and destroy foreign invaders is scarcely apparent in your daily life. However, it is this battle that is vital to your survival and the survival of the human species. New and terrifying microbes regularly emerge to challenge your immune system. Isn’t it comforting to know that you have “a magic doctor” present in your body?
The lymphatic system helps to maintain the balance of fluids in your body as well as containing white blood cells that seek and destroy invading pathogens. Your body has three lines of defence.
First, there are physical and chemical barriers, such as skin and stomach acid, that will prevent pathogens from harming healthy cells.
Second, there is a cell-mediated response. This response relies on macrophages, neutrophils, monocytes, and T-cells to recognize and destroy invading pathogens. Antigens, on the surface of the invading cells or on cells that pathogens—such as viruses—have invaded, identify them for destruction.
The third line of defence is the antibody-mediated response. Helper T-cells identify an invading pathogen and stimulate B-cells to produce antibodies. Antibodies are released into the blood and bind to specific antigens. Antibodies for salmonella will only work on the antigens on the surface of salmonella molecules.
Once antibodies have bound to invading antigens, three things can happen. The invading pathogen will be neutralized, the antibody can attract macrophages to destroy the pathogen, and/or the antibody will stimulate granulocytes and killer T-cells to release toxic molecules that will ultimately destroy the pathogen. Any large immune response to pathogens will exhibit a variety of symptoms such as fever, swelling, pus, and redness.
You may want to revisit the first video in this lesson as it provides a good summary of the immune system.
Lesson Glossary
cell-mediated immunity: involves the activation of white blood cells, specifically macrophages, neutrophils, monocytes, and T-cells rather than the production of antibodies
helper T-cell: arises from the thymus
These T-cells recognize an antigen on the surface of an invading pathogen and stimulate B-cells to produce antibodies.
killer T-cell: also known as a cytotoxic T-cell
It kills other target cells, such as cells infected with viruses, parasites, or cancer. These T-cells monitor all the cells of the body and are ready to destroy any cells that express foreign antigen fragments on the surface.
memory T-cell: a lymphocyte that carries receptors for a specific foreign antigen encountered in an earlier infection or through vaccination; it quickly promotes an immune response if the same antigen is re-encountered in a subsequent infection
suppressor T-cell: slows and suppresses the process of cellular immunity to ensure that normal tissue does not get destroyed
1.35. Lesson 6 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 6—Blood Types and Rh Factors
 Get Focused
Get Focused
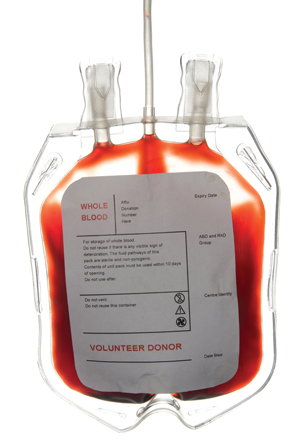
© Timothey Kosachev/shutterstock
Do you know what your blood type is? Have you or someone you know ever donated blood? In order for your donation to be used properly, medical professionals will determine your blood type when you decide to donate blood. How can they correctly identify your blood type?
In this lesson you will explore the following essential question:
- How do antigens identify blood types and Rh factors?
 Module 8: Lesson 6 Assignment
Module 8: Lesson 6 Assignment
Your teacher-marked Module 8: Lesson 6 Assignment requires you to submit a response to the following:
- TR 1. Identifying an Unknown Blood Type
You can access your Module 8: Lesson 6 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all the questions and place those answers in your course folder.
1.36. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Read
Read
Blood Typing
The ABO blood typing system is dependent on the presence or absence of different antigens on the cell membranes of the erythrocytes. Individuals with A, B, AB, or O blood types have different antibodies, or none at all, in their plasma depending on their blood type. For a successful blood transfusion to occur, the compatibility of the recipient’s and the donor’s blood must be determined. Some people are universal blood donors, while some people are universal blood recipients.
 Watch and Listen
Watch and Listen
You have the choice of viewing an animation that explains the difference between each of the blood types or looking at a slide show. Both provide an opportunity for a self-assessment of your understanding. If you are still unclear about blood typing, or you had difficulty with the
self-assessments, go to page 296 in the textbook for a written explanation. Or you can view the other media.
Animation
This animation explains the difference between each blood type. It also indicates what happens when different blood types mix.
After watching the animation, answer the five questions relating to ABO blood typing found below the animation. When you have completed the questions, click the “Submit Answers” button to get immediate feedback. If you answered a question incorrectly, the feedback will help you understand the correct response.
This slide show will walk you through the blood-typing process.
 Self-Check
Self-Check
SC 1. Complete this Self-Check activity about antigens.
 Try This
Try This
TR 1. Identifying an Unknown Blood Type
Given a scenario, you will describe a step-by-step procedure on how a student would identify four blood types.
Go to your Lesson 6 Assignment to complete this activity.
1.37. Page 3
Module 8—Circulation, Immunity, and Excretion
 Read
Read
The Rh System
In addition to the ABO blood-typing system, the presence or absence of the Rh factor (antigen) determines if an individual is Rh positive or Rh negative. An Rh+ individual has the Rh antigen on his or her blood cells, while an Rh- individual will lack Rh antigens. The Rh system was named after the rhesus monkey, since these monkeys were used to research blood typing.
A problem can arise if Rh- individuals are exposed to Rh+ blood. This typically happens when a pregnant woman (Rh-) gives birth to a baby who carries the Rh antigen because blood often mixes during childbirth. Once the mother is exposed to Rh+ blood, her body will identify this blood as a foreign substance and create Rh+ antibodies.
In possible subsequent pregnancies, where a baby is again Rh+, the mother’s antibodies may cross the placenta and endanger the child. A condition referred to as hemolytic disease of the newborn (HDN) can occur.
The Rh+ antibodies from the mother will begin destroying the baby’s blood cells and can lead to brain damage, deafness, and death. A series of diagrams on page 297 of the textbook illustrates and explains the mechanism of Rh incompatibility.
 Self-Check
Self-Check
Use the following information to answer the next two questions.
ABO Blood Type System and The RH System
Individual |
Antigen on Red Blood Cells |
Antibodies in Plasma |
Rh factor |
A |
A and B |
none |
Rh+ |
B |
none |
A and B |
Rh- |
C |
A |
anti-B |
Rh+ |
D |
B |
anti-A |
Rh- |
SC 2. Which individual in the chart above would have Type O negative blood?
- Individual A
- Individual B
- Individual C
- Individual D
SC 3. All of the individuals identified in the chart above are females, all had previous pregnancies with men who are Rh+, and all become pregnant a second time. Which individuals in the chart would have to be concerned about hemolytic disease of the newborn (HDN)?
- Individuals A and C
- Individuals A and B
- Individuals B and D
- Individuals C and D
 Self-Check Answers
Self-Check Answers
SC 2. B
SC 3. C
1.38. Page 4
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect
Reflect and Connect
Suppose your blood type was AB-. What would the tests, as shown in the blood-typing slide show, look like for this blood type? Explain the three different test results.
Identify what type of blood you could accept in a blood transfusion. You can review the slide show in order to complete this question. Save your response in your course folder. Being able to identify blood types is a skill that you will be tested on in an exam situation.
 Module 8: Lesson 6 Assignment
Module 8: Lesson 6 Assignment
Remember to submit the Assignment answers to your teacher as part of your Lesson 6 Assignment.
1.39. Page 5
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following essential question:
- How do antigens identify blood types and Rh factors?
By watching an animation and viewing a slide show, you have seen how antigens on the surface of a blood cell will identify your blood type. To determine blood types, blood must react with serums containing antibodies.
A reaction resulting in a clump of blood indicates a positive test for a particular antigen. Blood cells can contain A, B, and Rh antigens, while blood plasma can contain A, B, and Rh antibodies. Mixing blood types can result in an immune response that will kill blood cells. This is why blood donors and pregnant women are screened for blood type. It is a good idea to also know your own blood type for the benefit of medical professionals who may need to give you a blood transfusion in an emergency.
Lesson Glossary
Rh factor: a group of antigens found in most red blood cells; people with Rh antigen on their blood cells are Rh+
1.40. Lesson 7 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 7—Structures and Functions of the Excretory System
 Get Focused
Get Focused

© Alex Nikada/iStockphoto
Sometimes you just have to go to the washroom. Your body has devised a complex filtering system to clean your blood of metabolic wastes. Similarly, water treatment plants will filter wastes from water through a series of filtration processes. As a result, there is a waste product that has to be disposed. How is the human body designed to rid itself of metabolic wastes dissolved in blood?
In this lesson you will explore the following questions:
-
What are the principal structures of the excretory system, and how do they function?
-
How do nephrons contribute to the function of the excretory system?
 Module 8: Lesson 7 Assignment
Module 8: Lesson 7 Assignment
Your teacher-marked Module 8: Lesson 7 Assignment requires you to submit a response to the following:
-
TR 1. Investigation 9.A: Identifying Structures of the Excretory System
You can access your Module 8: Lesson 7 Assignment. You can print off the assignment or save the download to your computer. Your answers can be saved on this document to your course folder.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all the questions and place those answers in your course folder.
1.41. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Read
Read
The Problem of Wastes
Like any factory, the process of fabrication produces waste. Are you aware of all the types of wastes produced by the human body beyond the obvious ones?
You will have already learned that cellular respiration metabolizes glucose, resulting in carbon dioxide and water as the waste products. The respiratory system is the primary way that the body removes cellular respiration wastes (carbon dioxide and water). As protein is metabolized in the liver, toxic nitrogenous wastes such as ammonia, urea, and uric acid are produced. To avoid a buildup of these toxic wastes, mammalian vertebrates have evolved a complex excretory system.
Getting Rid of the Wastes from Proteins
Since the modern human diet is typically rich in protein, you often take in more protein than is required for growth and repair. Because of this excess, proteins are broken down, or metabolized, and transformed into carbohydrates or fats for energy storage. During protein metabolism, the amino group (NH2) from amino acids is removed by enzymes found in the liver. This process, called deamination, results in the formation of a toxic by-product called ammonia (NH3).
Ammonia is so toxic it cannot be stored for any time in the body; so, it must be converted into a less harmful form. This form is usually urea, which becomes a compound in urine. The formation of urea occurs when ammonia combines with carbon dioxide, also in the liver. Another nitrogenous waste that is formed primarily from the breakdown of certain nucleic acids is uric acid. Look at the series of graphics that show the creation of urea once an amino acid has been deaminated by an enzyme.
1.42. Page 3
Module 8—Circulation, Immunity, and Excretion
Structures of the Excretory System
So, what are the structures of the excretory system that will get rid of wastes and perform filtration?
kidneys: two organs that filter wastes from the blood and adjust the concentration of salts in the blood
The waste is excreted in the urine.
bladder: the organ where urine is stored before being discharged by the urethra
ureter: in mammals, a pair of muscular tubes that carry urine from the kidneys to the bladder
urethra: the tube through which urine exits the bladder and the body
The human excretory system is characterized by two kidneys located symmetrically in the lower abdominal region on either side of the spinal cord. The kidneys are the body’s blood cleaners.
The renal artery brings oxygenated blood to the kidney, while the renal vein removes deoxygenated blood. These two blood vessels deliver and move the large volume of blood necessary for efficient removal of the waste products. Each kidney is connected to the bladder by a long tube called the ureter.
The kidneys release urine through the ureters. The bladder stores urine and physically excretes urine to the external environment through another shorter tube called the urethra.
You may read pages 306 and 307 in the textbook and see visual diagrams.
 Try This
Try This
TR 1. Investigation 9.A: Identifying Structures of the Excretory System
You now have the opportunity to either perform a real dissection of a sheep’s kidney or observe a virtual dissection of a sheep’s kidney.
If you have access to the materials listed on page 309 of the textbook, you can proceed to complete the dissection as outlined.
Or you may choose to watch a virtual dissection.
In either case, you will go to your Lesson 7 Assignment to complete two analysis questions based on your experiences with the sheep’s kidney.
Look at the top of page 307 of the textbook for a labelled diagram of the excretory system.
 Read
Read
Kidney Structure and General Function
nephron: a microscopic tube-like filtration unit found in the kidneys that filters and reabsorbs various substances with the blood and produces urine
The main function of the kidneys is to filter, reabsorb, and secrete hormones. Filtration and reabsorption take place in the nephron, while kidney secretions are a function of the hormone system.

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007). 307, fig. 9.3. Reproduced by permission.
The nephron has three functional regions. Review these regions as described on page 308 of your textbook. Try the following Self–Check activity.
 Self-Check
Self-Check
SC 1. Complete this Self-Check activity.
 Module 8: Lesson 7 Assignment
Module 8: Lesson 7 Assignment
Remember to submit the Assignment answers to your teacher as part of your Lesson 7 Assignment.
1.43. Page 4
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following questions:
- What are the principal structures of the excretory system, and how do they function?
- How do nephrons contribute to the function of the excretory system?
The principal structures of the excretory system are the kidneys, ureter, urethra, bladder, renal vein, and renal artery. The kidneys are the filtering/absorbing workstation of this system, while renal blood vessels transport filtered and unfiltered blood to the kidneys. The ureter and urethra are also transport tubes that transfer urine to the bladder and the external environment.
Millions of functional units called nephrons within the kidneys are the site of filtration and absorption. Nitrogenous wastes such as urea, ammonia, and uric acid are filtered from the blood to form urine. The excretory system regulates homeostasis by maintaining blood composition and ridding the body of wastes.
In Lesson 8 you will further explore how the kidneys maintain the composition of the blood plasma by excreting metabolic wastes.
Lesson Glossary
bladder: the organ where urine is stored before being discharged by the urethra
kidneys: two organs that filter wastes from the blood and adjust the concentration of salts in the blood
The waste is excreted in the urine.
ureter: in mammals, a pair of muscular tubes that carry urine from the kidneys to the bladder
urethra: the tube through which urine exits the bladder and the body
1.44. Lesson 8 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 8—Urine Formation in the Nephron
 Get Focused
Get Focused

© Elenhil/shutterstock
While the filtration system of a water treatment plant may seem quite sophisticated with the removal of solids, as well as the processes of purification and disinfection, it is in reality much less so than the human filtration system.
Water treatment plants do not have millions of filtering tubes as there are in the kidney. However, they are similar in the sense that movement of the water through a filter is dependent on varying fluid pressures and the permeability or size of the filter. This is the same concept for the filtering of water and various components in and out of blood by the human kidney.
The glomerular ball accepts components out of the circulatory system forming the filtrate or what remains. The filtrate is then processed by the nephron to reabsorb into the blood valuable materials the body can use. Other materials left in the nephron form waste materials.
The water treatment plant continuously produces wastes and clean water as the products of its process. Urine formation by the kidneys is also a continuous process—it occurs independent of conscious thought. The unrelenting nature of this physiological activity requires you to release this liquid by-product of metabolism as it constantly builds up in the bladder.
At some point in a normal day, you have to urinate, whether it’s convenient or not. The excretory system recycles and reabsorbs what the body can use and removes waste materials the body can’t use.
In this lesson you will explore the following questions:
- How does the nephron function in maintaining the composition of blood plasma?
- How do the kidneys function in excreting metabolic wastes and expelling them into the environment?
 Module 8: Lesson 8 Assignment
Module 8: Lesson 8 Assignment
Your teacher-marked Module 8: Lesson 8 Assignment requires you to submit a response to the following:
- TR 1. Glomerular Filtration
- TR 2. Tubular Reabsorption
1.45. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Read
Read
Before you begin this lesson, you may want to read pages 311 to 315 of the textbook. The diagrams on these pages are useful in helping you to visualize the process of urine formation.
Urine Formation

© Tootles/shutterstock
Everyone depends on the process of urination for the removal of certain waste products in the body. The production of urine is vital to the body’s health. You have probably never thought of urine as valuable, but you could not survive if you did not produce it and eliminate it.
Urine is composed of water, certain electrolytes, and various waste products filtered out of the blood system. Remember, as blood flows through the body, wastes resulting from the metabolism of foodstuffs in the body cells are deposited into the bloodstream. This waste must be disposed of in some way.
Also, blood cells have a life of only about four months and, as they die, the cells are broken down. The yellow colour of urine comes from the breakdown of blood cells that is considered a waste to remove from the body.
A major part of this "cleaning" of the blood takes place in the kidneys and, in particular, in the nephrons, where the blood is filtered to produce the urine. Both kidneys in the body carry out this essential blood cleansing function. Normally, about one-fifth of the total blood pumped by the heart each minute will enter the kidneys to undergo filtration. The rest of the blood (about 80%) does not go through the filtering portion of the kidney. This blood flows through the rest of the body to serve the various nutritional, respiratory, and other needs that are always present.
There is more to the production of urine than the kidneys simply picking waste products out of the bloodstream and sending them along for final disposal. The kidneys two million or more nephrons (about a million in each kidney) form urine by three precisely regulated processes: filtration, reabsorption, and secretion.
Review the diagram of a simplified nephron to visualize the steps involved in filtration to create urine.

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 311, fig. 9.4. Reproduced by permission.
You may also want to read the attached document that reviews the processes of diffusion, osmosis, and active transport.
Glomerular Filtration

© travis manley/shutterstock
Glomerular filtration moves water and solutes from blood plasma into the nephron. This filtered fluid is referred to as filtrate or what remains. The glomerular filtrate consists primarily of water, excess salts (primarily Na+ and K+), glucose, and a waste product of the body called urea. Urea is formed in the body to eliminate the very toxic ammonia products that are formed in the liver from amino acids. Since humans cannot excrete ammonia, it is converted to the less dangerous urea and then filtered out of the blood. Urea is the most abundant of the waste products that must be excreted by the kidneys.
The total rate of glomerular filtration for the whole body (i.e., for all of the nephrons in both kidneys) is normally about 125 mL per minute. That is, about 125 mL of water and dissolved substances are filtered out of the blood per minute. The following calculations may help you visualize how enormous this volume is:
125 mL/min X 60 min/hr = 7500 mL/hr or 7.5 L/hr = 180 L/day
Imagine the size of a 2-litre bottle of soda pop. About 90 of those bottles equals 180 litres! In your experience you have never excreted anywhere near 180 litres of urine per day. Why? Because almost all of the estimated 180 litres of water that leaves the blood through glomerular filtration—the first process in urine formation—returns to the blood by the second process of reabsorption.
glomerulus: a fine network of capillaries within Bowman’s capsule arising from the renal artery
Bowman’s capsule: a caplike formation at the top of each nephron that serves as a filtration structure; surrounds the glomerulus
Filtration occurs because of two factors. Firstly, the blood pressure in the glomerulus is four times greater than in other capillaries in the body. This creates a force against capillary walls that aids in moving water and solutes from the blood to Bowman’s capsule. Secondly, the glomerulus’ capillaries are quite permeable. Thus, small molecules (including water, NaCl, glucose, urea, and certain amino acids) are forced into Bowman’s capsule. Larger proteins and red blood cells are left behind in the arteriole leading away from the glomerulus. If protein or blood is found in urine, this indicates a problem.
 Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 311, fig. 9.4. Reproduced by permission.
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 311, fig. 9.4. Reproduced by permission.
 Try This
Try This
TR 1. Glomerular Filtration
Urine formation occurs as blood pressure forces filtrate from the glomerulus into Bowman’s capsule. This bulk flow of fluids into the Bowman’s capsules of the nephrons in both kidneys creates about 180 L of filtrate per day. All but about 1 L will be actively reabsorbed back into the blood, with a great expenditure of ATP.
Go to your Lesson 8 Assignment to respond to how this process will work.
1.46. Page 3
Module 8—Circulation, Immunity, and Excretion
 Read
Read
Tubular Reabsorption

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 312, fig. 9.5. Reproduced by permission.
Filtrate from the glomerulus moves to Bowman’s capsule. From there, the filtrate moves along the proximal tubule where the filtrate is reabsorbed from the proximal tubule through active and passive transport mechanisms (diffusion, osmosis).
Reabsorption, by definition, is the movement of substances out of the renal tubules back into the blood capillaries located around the tubules. The nutrient glucose (blood sugar) is entirely reabsorbed back into the blood from the proximal tubules. Glucose is actively transported out of the tubules and into the capillary net that surrounds the tubule.
None of this valuable nutrient is wasted by being lost in the urine. However, even when the kidneys are operating at peak efficiency, the nephrons can reabsorb only so much sugar and water. Their limitations are dramatically illustrated in cases of diabetes mellitus, a disease which causes the amount of sugar in the blood to rise far above normal.
As already mentioned, in ordinary cases all the glucose that seeps out through the glomeruli into the tubules is reabsorbed into the blood. But if too much glucose is present, the tubules reach the limit of their ability to pass the sugar back into the bloodstream, and the tubules retain some of it. It is then carried along in the urine, often providing a doctor with her first clue that a patient has diabetes mellitus.
The value of urine as a diagnostic aid has been known to the world of medicine since as far back as the time of Hippocrates. Since then, examination of urine has become a regular procedure for physicians as well as for scientists.
proximal tubule: the tubule connected to Bowman’s capsule
Its main function is the reabsorption of water and solutes as well as the secretion of hydrogen ions.
distal tubule: the tubular portion of the nephron that lies between the loop of Henle and the proximal tubule
The distal tubule’s main function is the reabsorption of water and solutes and the secretion of various substances.
loop of Henle: a tubular portion of the nephron
It is an extension of the proximal tubule that loops into the medulla of the kidney and its main function is the reabsorption of water and ions.
The descending loop of Henle reabsorbs mostly water and some ions. The medulla region of the kidney is a salty environment. The cells of the descending loop are permeable to water and only slightly permeable to ions. Therefore, mostly water leaves the filtrate to return to the blood. The concentration of Na+ increases towards the bottom of the loop.
The ascending loop of Henle becomes impermeable to water and slightly permeable to solutes. Sodium ions diffuse from the filtrate to nearby blood vessels. The top of the ascending loop becomes thick walled and ions are transported via active transport. This reduces the concentration of the filtrate and replenishes the salty environment of the medulla.
The distal tubule reabsorbs sodium ions, chloride ions, and water depending on the needs of the body. As a person increases the amount of salt taken into the body, the kidneys decrease the amount of sodium reabsorption back into the blood. That is, more sodium is retained in the tubules. Therefore, the amount of salt excreted in the urine increases. The process works the other way as well. The less the salt intake, the greater the amount of sodium reabsorbed back into the blood, and the amount of salt excreted in the urine decreases.
Tubular Secretion
Secretion is the process by which substances move into the distal and collecting tubules from blood in the capillaries around these tubules. Secretion is reabsorption in reverse.
Whereas reabsorption moves substances out of the tubules and into the blood, secretion moves substances out of the blood and into the tubules where they mix with the water and other wastes and are converted into urine. These substances are secreted through either an active transport mechanism or as a result of diffusion across the membrane.
Substances secreted are hydrogen ions (H+), potassium ions (K+), urea, and certain drugs. Potassium (K+) and hydrogen (H+) ions are actively transported into the distal tubule from the capillaries. Potassium in certain concentrations must be maintained as it is required to transmit nerve impulses. Hydrogen ions need to be balanced in order to maintain blood pH. Too many hydrogen ions in the blood can create an acidic environment, which inhibits cellular function.
Collecting Duct Reabsorption
Adapted from Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), BLM 9.2.2. Reproduced by permission.
Once the filtrate has moved through the entire proximal tubule (loop of Henle), it enters the collecting duct. The collecting duct extends into the salty environment of the medulla. This causes water to move across the tubule membrane by osmosis.
If a person is dehydrated, the collecting duct becomes more permeable to water and more water is reabsorbed in order to conserve water. This process is controlled by hormones. You will explore the role of hormones in Lesson 9. Finally, the filtrate, which is about 1% of the original volume, is now urine and is ready to be moved by the ureters to the bladder.
 Try This
Try This
TR 2. Tubular Reabsorption
Solutes are actively and passively transported from the filtrate in the proximal tubule back into the blood. Go to your Lesson 8 Assignment to complete an activity that tests your knowledge of how filtrate moves through the proximal tubules of the kidney.
1.47. Page 4
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect
Reflect and Connect
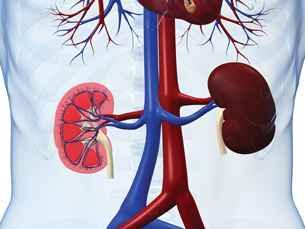
© Sebastian Kaulitzki/shutterstock
Your body is incredibly efficient at filtering blood. The sheer volume of blood filtered by the kidneys is extraordinary considering that a kidney is the size of a conventional computer mouse.
Water treatment plants in Edmonton produce about 530 million litres of filtered water every day. To put your kidneys in perspective, think of this: Water treatment plants service approximately 1 million people. This means that 530 L of water is filtered per person per day.
Water treatment plants are huge. Your kidneys, each the size of a computer mouse, process 180 L blood per day for one person. This size difference illustrates the efficiency of your body to filter blood and create urine. Complete the following questions to test your knowledge.
 Self-Check
Self-Check
SC 1. Complete this Self-Check activity.
 Module 8: Lesson 8 Assignment
Module 8: Lesson 8 Assignment
Remember to submit the Assignment answers to your teacher as part of your Lesson 8 Assignment.
1.48. Page 5
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following questions:
- How does the nephron function in maintaining the composition of blood plasma?
- How do the kidneys function in excreting metabolic wastes and expelling them into the environment?
Three processes occurring in successive portions of the nephron accomplish the function of urine formation:
- Filtration of water and dissolved substances out of the blood in the glomeruli and into Bowman's capsule by arteriole blood pressure and passive transport.
- Reabsorption of water and dissolved substances from the filtrate out of the kidney tubules (proximal, loop of Henle, distal, and collecting duct) back into the blood occurs through passive and active transport. This process prevents substances needed by the body from being lost in the urine. The proximal tubule actively reabsorbs nutrients such as glucose and positively charged ions (Na+), while passively reabsorbing water and negatively charged ions (Cl-). The main function of the descending loop of Henle is to reabsorb water through osmosis. The main function of the ascending loop of Henle is to reabsorb sodium ions. Active reabsorption of sodium ions occurs in the distal tubule, while negative ions and water are passively reabsorbed.
- The secretion of hydrogen ions (H+), potassium ions (K+), urea, and certain drugs out of the blood and into the kidney tubules occurs through passive and active transport. The proximal and distal tubules actively transport hydrogen ions from the blood, while urea and potassium ions move passively. These molecules are eventually eliminated in the urine.
Lesson Glossary
Bowman’s capsule: a caplike formation at the top of each nephron that serves as a filtration structure; surrounds the glomerulus
distal tubule: the tubular portion of the nephron that lies between the loop of Henle and the proximal tubule
The distal tubule’s main function is the reabsorption of water and solutes and the secretion of various substances.
glomerulus: a fine network of capillaries within Bowman’s capsule arising from the renal artery
loop of Henle: a tubular portion of the nephron
It is an extension of the proximal tubule that loops into the medulla of the kidney and its main function is the reabsorption of water and ions.
proximal tubule: the tubule connected to Bowman’s capsule
Its main function is the reabsorption of water and solutes as well as the secretion of hydrogen ions.
1.49. Lesson 9 Intro
Module 8—Circulation, Immunity, and Excretion
Lesson 9—Maintaining the Excretory System
 Get Focused
Get Focused
After drinking a thirst-quenching glass of water, have you ever considered that a water treatment plant determines specific levels of minerals and ions acceptable for tap water? Since water is essential for humans to drink, having too many chemicals and salts in water is not healthy.
Water treatment plants take this into account and try to balance the chemicals necessary to make water safe to drink, yet healthy for humans to drink.
Your kidneys play a similar role. The kidneys ensure that your water and ion levels are maintained. How do the kidneys react if you drink too much or too little water?
In this lesson you will explore the following questions:
- How do the kidneys contribute to homeostasis in terms of water and ions?
- How does the design of the kidney relate to dialysis technologies?
 Module 8: Lesson 9 Assignment
Module 8: Lesson 9 Assignment
Your teacher-marked Module 8: Lesson 9 Assignment requires you to submit a response to the following:
- TR 1. Maintaining Homeostasis
- Lab: Urinalysis
- TR 2. Hemodialysis and Peritoneal Dialysis
1.50. Page 2
Module 8—Circulation, Immunity, and Excretion
 Explore
Explore
 Read
Read
The body’s water or osmotic balance is critical to the maintenance of blood plasma solute concentration and blood volume. Both of these factors play roles in the movement of materials between the cells and the blood as well as blood pressure. When the balance between blood volume and blood plasma solute concentration are disrupted, the body’s systems may begin to fail, with possible disastrous consequences.
Water intoxication is an interesting example of how your body can react to imbalance. Water intoxication occurs when the normal balance of electrolytes in the body become severely altered due to an excess of water consumption. This can impair brain function much like alcohol, but for different reasons.
The concentration gradient between ions such as sodium and outside cells is lowered. Osmotic pressure is reversed and water moves into the cells in an effort to balance concentration. Electrolyte imbalance and tissue swelling can cause fluid in the lungs and an irregular heartbeat. Swelling puts pressure on the brain and nerves, which can produce behaviour resembling alcohol intoxication. Water intake must be restricted and an electrolyte solution given to someone suffering from water intoxication before swelling causes too much damage.
dehydration: a relative deficiency of water molecules in relation to other dissolved solutes; can be caused by blood loss, vomiting, excess exertion, or malnutrition
hypothalamus: a gland located above the brain stem and connects the nervous system with the endocrine system by relaying messages to the pituitary gland; it is the size of an almond
osmoreceptors: a sensor found in the hypothalamus of the brain that detects changes in osmotic pressure
antidiuretic hormone: a hormone in all mammals that stimulates increased water reabsorption by the kidneys; also called vasopressin
Instances of water intoxication are much less common than the opposite extreme of dehydration. Your body has a mechanism to respond to high osmotic pressure in your bloodstream that occurs under dehydrated conditions. High osmotic pressure occurs when there is low water and high solute (salt) concentrations.
Osmotic pressure is controlled by the hypothalamus and its interaction with the posterior pituitary gland of the brain. The hypothalamus contains osmoreceptors. Osmoreceptors detect osmotic pressure. If osmotic pressure is high, the pituitary is stimulated to release a hormone called antidiuretic hormone, or ADH. ADH increases the permeability of the distal tubule and collecting duct of the nephron to water. ADH is sometimes referred to as vasopressin due to its secondary effect of causing a moderate increase in blood pressure through vasoconstriction. By increasing the permeability of these regions of the nephron, water is reabsorbed back into the bloodstream. This lowers the osmotic pressure—a negative feedback effect.
A simple feedback loop showing this interaction can be illustrated as follows.
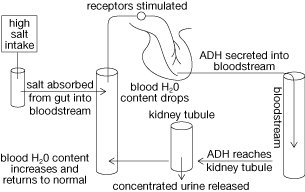
diabetes insipidus: a condition characterized by the excretion of large amounts of severely diluted urine, which cannot be reduced when fluid intake is reduced
It denotes an inability of the kidney to concentrate urine. DI is caused by a deficiency of antidiuretic hormone (ADH), also known as vasopressin.
A number of circumstances can decrease ADH release from the pituitary. Individuals with diabetes insipidus are unable to produce sufficient quantities of ADH to allow for normal water reabsorption. These people release large quantities of dilute urine, leading to dehydration. The consumption of alcoholic beverages, as well as caffeinated drinks, temporarily blocks the release of ADH. This also leads to increased urine output and subsequent dehydration.
 Self-Check
Self-Check
SC 1. What is the role of osmoreceptors in regulating water reabsorption?
SC 2. What is the role of ADH in maintaining the volume of water in the body?
 Self-Check Answers
Self-Check Answers
SC 1. Osmoreceptors are sensitive to osmotic pressure and will stimulate or inhibit the release of ADH from the pituitary.
SC 2. ADH increases the permeability of the distal tubule and the collecting duct to allow more water to be reabsorbed into the blood. ADH is secreted under conditions of dehydration so that your body conserves water.
 Read
Read
The Reabsorption of Salts
aldosterone: a hormone that causes the tubules of the kidneys to retain sodium and water
This increases the volume of fluid in the body, and drives up the blood pressure.
The kidneys reabsorb Na+ or sodium ions at the proximal tubule of the nephron. A further reabsorption of Na+ also occurs at the distal tubule and collecting duct when Na+ levels in the bloodstream drop abnormally. This secondary Na+ reabsorption may also be related to a drop in blood pressure and is under the control of the hormone aldosterone.
What happens when blood pressure drops or Na+ concentration in the blood is reduced? Receptors found in the kidney release an enzyme called renin. Renin converts another enzyme, angiotensinogen, to its active form of angiotensin. Angiotensin causes a constriction of blood vessels and increases the thirst sensation. At the same time, it stimulates the release of aldosterone from a triangular-shaped gland located on top of each kidney.
Aldosterone stimulates the distal tubules and collecting ducts to reabsorb Na+. Negatively charged chlorine ions and water are also reabsorbed, which has the net effect of retaining salt and water. Aldosterone also stimulates the secretion of K+ into the distal tubes and collecting ducts if the concentration of potassium ions in the blood is high.
 Try This
Try This
TR 1. Maintaining Homeostasis
You will be given a variety of situations and you will conduct research and create a flow chart to describe how humans maintain homeostasis with respect to water and ions.
Go to your Lesson 9 Assignment for further instructions.
1.51. Lab
Module 8—Circulation, Immunity, and Excretion
 Lab: Urinalysis
Lab: Urinalysis
You will now perform a modified urinalysis based on the investigation on page 320 of your textbook.
Problem
What physical and chemical tests can you use, and what data do they provide in the analysis of urine?
Procedure
Consider this scenario. A theft was committed in the washroom of a community building. Forensic specialists collected a urine sample at the scene of the crime. The police have four suspects in custody. Your task is to find out who committed the crime.
Open the Lesson 9 Assignment file, where there is a table to document the results of the tests and support the elimination of suspects. For each test, indicate the results for each individual in the chart. Once you have recorded the results for all of the tests, you should be able to identify the criminal.
You will start by interpreting the results of each test.

© Christina Richards/iStockphoto
Test 1—Colour, Odour, Clarity: Normal urine is a clear, straw-coloured liquid. Urine may be cloudy because it contains red or white blood cells, bacteria, or pus from a bladder or kidney infection. Normal urine has a slight odour. Foul-smelling urine is a common symptom of a urinary tract infection. A fruity odour is associated with diabetes mellitus. Use the following descriptions of the urine samples to fill in your chart located in your Lesson 9 Assignment.
Control: Urine is yellow. Smell is normal. Looks cloudy.
Crime suspect: Urine is yellow. Smell is fruity. Looks clear.
Suspect 1: Urine is yellow. Smell is fruity. Looks clear.
Suspect 2: Urine is yellow. Smell is normal. Looks clear.
Suspect 3: Urine is yellow. Smell is normal. Looks cloudy.
Suspect 4: Urine is yellow. Smell is fruity. Looks clear.

© mypokcik/shutterstock
Test 2—Protein: One sign of kidney damage is the presence of protein in urine. To test for protein, a portion of each sample is placed in a hot water bath. If the sample becomes cloudy or is cloudier than the original sample, it contains protein.
- After a few minutes, the test tube from the hot water bath is removed and compared to the original sample.
- If the heated sample is cloudier, it contains protein. The test is positive.
Use the following descriptions of the urine samples to fill in your chart located in your Lesson 9 Assignment.
Control: positive
Crime Suspect: negative
Suspect 1: negative
Suspect 2: negative
Suspect 3: positive
Suspect 4: negative
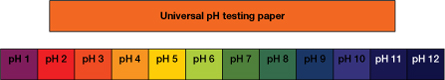
Test 3—pH: The wide range of pH values (pH 4.7 to 8.5) makes this the least useful parameter for a diagnosis of kidney disorders. Kidney stones are less likely to form and some antibiotics are more effective in alkaline urine. There may be times when acidic urine may help prevent some kinds of kidney stones. Bacterial infections also increase alkalinity, producing a urine pH in the higher 7–8 range.
A clean medicine dropper is used to place a drop of each sample of urine on small pieces of universal indicator (pH) paper. They are left for about 30 seconds. The pH paper can turn several different shades, depending on pH. pH can be determined by comparing the indicator to a colour chart.
Use the following descriptions of the urine samples to fill in the chart located in your Lesson 9 Assignment. To determine pH, use this indicator colour chart.
Control: yellow green
Crime Suspect: yellow/green
Suspect 1: orange
Suspect 2: green/blue
Suspect 3: green
Suspect 4: yellow/green

© Norman Chan/shutterstock
Test 4—Glucose: One sign that a person has diabetes mellitus is the presence of glucose in the urine.
- To test for glucose, a glucose test strip is dipped into each sample of unheated urine and immediately taken out.
- The strip is compared to a colour chart. The chart shows a colour gradient from light blue to dark brown. Intermediate colours are greens and browns. Blue indicates no sugar, while dark brown indicates high glucose levels. Intermediate colours indicate the presence of glucose in varying concentrations.
Use the following descriptions of the urine samples to fill in your chart located in your Lesson 9 Assignment.
Control: dark brown
Crime Suspect: dark brown
Suspect 1: light blue
Suspect 2: green
Suspect 3: light blue
Suspect 4: dark brown
From the results of the urine analysis, you should be able to tell which suspect committed the crime, or at the very least left his or her urine at the crime scene.
Complete the Analysis questions in the Lesson 9 Assignment.
1.52. Page 4
Module 8—Circulation, Immunity, and Excretion
 Read
Read
Kidney Problems

© beerkoff/shutterstock
The excretory system can experience many different problems. You can experience urinary tract infections where your immune system and antibiotics will fight the infection. You can also experience kidney stones, a crystallization of excess calcium in the urine. These can be painful to excrete and may cause damage to the kidney.
Kidneys can also be damaged by kidney infections, high blood pressure, diabetes, or blunt force trauma to the lower back where the kidneys are located. Arteriosclerosis can reduce blood flow to the kidneys, and tubules can become blocked. Irreversible damage to the kidneys may require a person to undergo dialysis or a kidney transplant.
Dialysis is the diffusion of dissolved substances through a mechanical semipermeable membrane. Technology based on the same principles of filtration in the kidney has been developed to aid people with kidney disfunction.
Read pages 319 to 325 of the textbook to learn more about these problems and treatments.
 Self-Check
Self-Check
SC 3. One of the effects of mercury poisoning is the complete stoppage of the kidney function. What would be the first symptom of kidney function shutdown?
SC 4. With kidney failure, urea levels accumulate in the blood, affecting the absorption of water from the large intestine into the blood. Explain the effect of the high urea concentration in the plasma on water reabsorption in the large intestine and on the water balance in the body cells.
SC 5. After an episode of severe bleeding, the production of urine ceases temporarily. Identify the hormone involved, and describe its action in this situation.
SC 6. What hormone is involved in the homeostatic reabsorption of water from the urine in the kidney tubule?
 Self-Check Answers
Self-Check Answers
SC 3. Urine production would stop, so the person would not urinate. The body would swell due to the excess water in the body.
SC 4. There is an increasing amount of water absorbed by the intestine because the blood is becoming increasingly hypertonic with the increasing levels of urea in the blood. The water inside the cells diffuses into hypertonic blood, causing dehydration of the cells.
SC 5. The hormone aldosterone is secreted when blood volume drops. Aldosterone stimulates the distal convoluted tubule to reabsorb more salt, and water follows by osmosis. This leads to a drop in urine production.
SC 6. The hormone involved in the reabsorption of water by the tubule is ADH.
 Try This
Try This
TR 2. Hemodialysis and Peritoneal Dialysis
When kidney failure occurs, blood plasma is said to become uremic, because urea molecules accumulate to dangerous levels. Imbalances in other substances, such as salts and hydrogen ions, also occur.
Dialysis is a medical procedure in which the composition of the plasma can be corrected through simple diffusion. Dialysing fluid (dialysate) is separated from the patient’s blood (uremic plasma) by thin semi-permeable membranes. Molecules and ions diffuse into or out of the patient’s plasma, depending upon the composition of the dialysate. Thus, careful formulation of dialysate is the key to correcting the composition of uremic plasma.
In hemodialysis, diffusion occurs across artificial membranes. In peritoneal dialysis, it occurs across the intestinal lining (peritoneum). These procedures are illustrated.
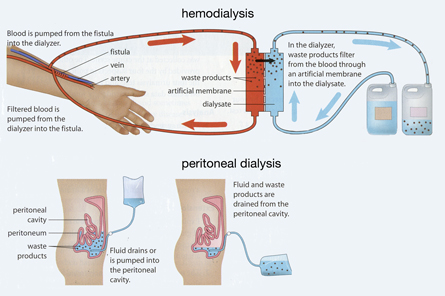
Adapted from Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), BLM 9.3.5. Reproduced by permission.
Go to your Lesson 9 Assignment to complete this activity.
 Discuss
Discuss
Organ donation, such as that necessary for kidney transplantation, is an often-misunderstood process. It is a process critical for the health and well-being of many Canadians. The number of available kidneys from donors is far less than those needed by individuals who have kidney disease. The desperation that those on waiting lists face often forces them to take drastic measures.
Do a web search to find out what lengths people will go to to prolong their lives by obtaining a new kidney. Post your findings in the discussion area and read other postings. Does the research surprise you? Jot down a few notes for your own information in your course folder.
1.53. Page 5
Module 8—Circulation, Immunity, and Excretion
 Reflect and Connect
Reflect and Connect
 Self-Check
Self-Check
SC 7. Complete this Self-Check activity.
You may also want to try working through Chapter Review questions on page 328 and 329 of the textbook. You should save your responses to your course folder for exam review. If you would like feedback on any of these questions, you may contact your teacher.
 Going Beyond
Going Beyond
As you can read on page 317 in the textbook, the maintenance of blood pH is a complex process that involves chemical buffering in the blood, regulation of the respiratory rate, and, most importantly, control of the excretion of H+ and the reabsorption of HCO3– at the kidney.
When the body is pushed to extremes by exercise, the acid-base equilibrium may be disrupted. Exercise increases the rate of cellular respiration and thus the breakdown of glucose and the subsequent production of CO2 as well as the generation of H+. These products cause the blood pH to drop below its normal value of 7.4. This circumstance, known as acidosis, prevents many normal metabolic reactions from occurring and may even lead to death.
 Module 8: Lesson 9 Assignment
Module 8: Lesson 9 Assignment
Remember to submit the Assignment answers to your teacher as part of your Lesson 9 Assignment.
1.54. Page 6
Module 8—Circulation, Immunity, and Excretion
 Lesson Summary
Lesson Summary
In this lesson you explored the following questions:
- How do the kidneys contribute to homeostasis in terms of water and ions?
- How does the design of the kidney relate to dialysis technologies?
The kidneys maintain the water-salt balance in the body. Water balance is maintained when the body senses osmotic pressure via osmoreceptors. High or low pressures stimulate or inhibit the release of antidiuretic hormone (ADH). ADH causes the collecting ducts and distal tubules to become more permeable to water, thereby helping the body to conserve water when necessary.
Another hormone, aldosterone, regulates the amount of salt in the body by reabsorbing sodium ions. Aldosterone increases the permeability of the collecting duct and distal tubules for Na+. You discovered that urinalysis can be used as a tool to determine health conditions. Dialysis was presented to you as a treatment for kidney failure. Blood is filtered using principles of diffusion either internally (using your intestine) or externally (being hooked up to a machine).
Now that you are at the end of this module, you will complete your Module 8 project. For the module project you will have the choice between three extended responses. The purpose of an extended response is to help you take a closer look at a specific area of study. In the module project you will choose between investigating the heart, an immune response, or a disease of the kidney. You will find further information in your Module Summary.
Lesson Glossary
aldosterone: a hormone that causes the tubules of the kidneys to retain sodium and water
This increases the volume of fluid in the body, and drives up the blood pressure.
antidiuretic hormone: a hormone in all mammals that stimulates increased water reabsorption by the kidneys; also called vasopressin
dehydration: a relative deficiency of water molecules in relation to other dissolved solutes; can be caused by blood loss, vomiting, excess exertion, or malnutrition
diabetes insipidus: a condition characterized by the excretion of large amounts of severely diluted urine, which cannot be reduced when fluid intake is reduced
It denotes an inability of the kidney to concentrate urine. DI is caused by a deficiency of antidiuretic hormone (ADH), also known as vasopressin.
hypothalamus: a gland located above the brain stem and connects the nervous system with the endocrine system by relaying messages to the pituitary gland; it is the size of an almond
osmoreceptors: a sensor found in the hypothalamus of the brain that detects changes in osmotic pressure
1.55. Module Summary/Assessment
Module 8—Circulation, Immunity, and Excretion
 Module Summary
Module Summary
In this module you explored circulation, immunity, and excretion. The Big Picture connected these three body systems with the functioning of a water treatment plant. You explored the circulatory system in the first four lessons. Like a water treatment plant, the mechanics of a circulatory system include pumps, valves, tubing, and fluids. The primary structures of the circulatory system are the heart, veins, arteries, capillaries, and blood.
As you worked through each lesson you discovered how blood moves through the body, technologies related to the circulatory system, the components of blood, and how the circulatory system exchanges matter and energy with the environment.
By participating in a virtual dissection of a sheep’s heart, you were able to identify structures of the heart and map the flow of blood of pulmonary and systemic circulation. You explored the components and function of components in the blood—hemoglobin, plasma, and platelets.
Blood is a multifaceted component of your circulatory system that transports nutrients, gases, and wastes, contains cells for immunity, and has the ability to clot if you are injured. Energy flow is also maintained via the circulatory system. The ability for blood to absorb heat and the design of your network of blood vessels allows heat to be transferred or conserved in order to maintain body temperature. You also explored the importance of blood pressure as a mechanism to control the exchange of matter and as a measure of health.
In Lessons 5 and 6 you explored how your body deals with invading pathogens. As a water treatment plant removes harmful substances from tap water, your immune system also destroys harmful substances. You further explored the role of blood in immunity and you were introduced to the lymphatic system. Your body has three lines of defence against invading pathogens: physical/chemical barriers, cell-mediated response, and antibody mediated response.
Through a virtual blood typing activity, you discovered that blood type is dependent on antigens and antibodies. The wrong type of blood transfusion would create an immune response.
In the remaining lessons of this module you explored the excretory system. This is your body’s filtration system. Before tap water ends up in your glass, water has undergone several filtration processes to remove waste. Similarly, as blood cycles through your body, it is continually filtered by the kidneys. You studied the major structures of the kidney by following a virtual kidney dissection.
The nephrons were a major focus of the excretory system. As you investigated the structures of the kidney, you also examined how the nephrons regulate homeostasis by maintaining blood composition and ridding the body of wastes. You specifically looked at three processes occurring in successive portions of the nephron that form the waste products of urine: filtration, reabsorption, and secretion.
Lastly, you explored the role of the kidneys in maintaining the water-salt balance in the body. Via hormones, aldosterone, and ADH, electrolytes and osmotic pressure are controlled. Altering the permeability of the nephron to water and sodium ions helps to maintain homeostasis. You explored how urinalysis can be used to diagnose conditions such as diabetes mellitus. Technology, such as dialysis, has been developed to help people with kidney disorders. This technology mimics the filtration of blood across a semi-permeable membrane.
Each of the three systems studied in this module is dependent on the other ones. Without blood, the kidneys would have nothing to filter, the heart would have nothing to pump, and you would have no immunity. You would cease to exist as a living human being.
Without a heart, blood could not circulate, would not be filtered by the kidneys, would not be able to find pathogens, and would not transfer nutrients or gases. You would cease to exist.
Without kidneys your blood would remain unfiltered, and toxins would build up and inhibit the function of cells in the heart. You would cease to exist. There is a definite pattern. Homeostasis in your body hinges on the interdependence and health of all body systems.
Now that you have completed the lessons in this module, you will complete a module assessment project. In the module project you will have the choice between three extended responses. You will choose between investigating the circulatory system, the immune system, or the excretory system. You will also complete a final question that ties the three systems together. Once you have completed this module project, you will go to the Unit D Assessment.
Module Project
You will complete one of the three extended responses and a final question that ties together the three systems you studied. The purpose of an extended response is to help you take a closer look at a specific area of study. In this case you will choose between investigating the circulatory system, the immune system, or the excretory system. You may choose an assignment because you feel you have a stronger grasp of the content or you may choose an assignment because you feel you would benefit from a further study of that particular body system. The extended response activities allow you to further explore each body system. In the Unit Assessment you will build upon these module projects by pursuing an in-depth inquiry into the interdependence of your body systems in maintaining homeostasis.
Circulation
In this investigation you will explore the heart, related technology, and its function in the circulatory system. Your response may be presented as a written report, a diagram, a flow chart, a podcast, or in another format you have discussed with your teacher.
When a doctor listens to a patient’s heart with a stethoscope, sometimes swishing or whooshing sounds—called heart murmurs—are heard in addition to the standard “lub-dub” of the heartbeat. Heart murmurs result from the turbulent flow of blood through the heart—this is why they can sound like water rushing through the end of a garden hose. Pediatricians classify most heart murmurs they hear as innocent, because they are not associated with a heart disease or abnormality. Most children will have a heart murmur at some time, but these innocent murmurs usually disappear by the time they become adults.
The doctor may decide that the characteristics of a particular heart murmur require additional testing to determine if there is an underlying problem with blood flow through the heart. In these cases, the murmur is usually due to the abnormal functioning of a heart valve. A valve may not be closing tightly—it may be too narrow or too stiff. A treatment plan is then designed to address the specific condition.
- a) Draw a cross-sectional sketch of the human heart and label all of the chambers, valves, and major blood vessels that take blood into and away from the heart. (10 marks)
b) Use a flow chart or illustration to trace the flow of blood through the heart. Start with the blood in the inferior vena cava, and end with blood entering the aorta. Include all of the chambers, valves, and major blood vessels that take blood into and away from the heart. (6 marks)
c) Describe how you would use a stethoscope to determine damage to the aortic semilunar valve and damage to the left atrioventricular valve. Provide details, including what you would expect to hear and when in the cardiac cycle you would hear this particular sound. (4 marks)
d) Explain what is meant by the term pulse. (2 marks)
Immunity
In this investigation you will explore the immune response to an organ transplant. Your response may be presented as a written report, a diagram, a flow chart, a podcast, or in another format you have discussed with your teacher.
- Explain the immune response that resulted in tissue rejection of early heart transplants. (4 marks)
- Research the term immunosupression. Compare how the immune system would respond in a transplant patient given immunosuppressive drugs with a patient not given these drugs. (8 marks)
Excretion
In this investigation you will look at a disease of the kidney and the damage it will cause. Your response may be presented as a written report, a diagram, a flow chart, a podcast or in another format you have discussed with your teacher.
Use the information below to answer the next questions.
Glomerular Diseases
Glomerular diseases, such as glomerulonephritis, result in damage to the glomeruli in the nephrons of the kidney.
Signs and symptoms of glomerulonephritis may depend on whether one has the acute or chronic form, and the cause. The first indication that something is wrong may come from symptoms or from the results of a routine urinalysis. Signs and symptoms may include
- cola-coloured or diluted iced-tea-coloured urine from red blood cells in the urine (hematuria)
- foam in the toilet water from protein in the urine (proteinuria)
- high blood pressure (hypertension)
- fluid retention (edema) with swelling evident in the face, hands, feet, and abdomen
- fatigue from anemia or kidney failure
- less frequent urination than usual
- a) Explain how glomerular disease (glomerulonephritis) can result in high blood pressure and why high blood pressure can do further damage to the kidneys. (3 marks)
b) Explain why the urine of a healthy person does not contain protein or red blood cells, and describe how protein and red blood cells enter the urine of a person who has glomerulonephritis. (4 marks)
c) Explain how the hormone aldosterone raises blood pressure. (3 marks)
d) Define the term dialysis and describe the movement of dissolved substances. (3 marks)
e) Using a diagram or a sketch, explain how hemodialysis (artificial kidney) is used to purify the blood of a person who has end-stage renal disease. (6 marks)
f) Describe the impact on the life of a person who must undergo hemodialysis. (4 marks)
Final Question
You have been exposed to the German measles but luckily your inoculations (shots) are up to date. Your point of contact with the virus was the alveoli of the respiratory system. Trace from that point the movement of the virus through the circulatory system by naming and describing the major blood vessels and the chambers of the heart.
Describe how the immune system recognizes and attacks the foreign proteins of the virus. Describe how the virus is broken down and removed by the excretory system.
This path can be described or illustrated through a text or graphic response.
1.56. Module Glossary
Module 8—Circulation, Immunity, and Excretion
Module Glossary
aldosterone: a hormone that causes the tubules of the kidneys to retain sodium and water
This increases the volume of fluid in the body, and drives up the blood pressure.
antibody: a protein in the blood that identifies and neutralizes foreign invaders, such as bacteria or viruses
Each antibody is specific to a particular invader.
antidiuretic hormone: a hormone in all mammals that stimulates increased water reabsorption by the kidneys; also called vasopressin
arterial pressure: the pressure blood exerts on artery walls
bladder: the organ where urine is stored before being discharged by the urethra
Bowman’s capsule: a caplike formation at the top of each nephron that serves as a filtration structure; surrounds the glomerulus
cell-mediated immunity: involves the activation of white blood cells, specifically macrophages, neutrophils, monocytes, and T-cells rather than the production of antibodies
coagulation: the process where a damaged blood vessel wall is covered by a platelet and fibrin-containing clot to stop bleeding and begin repair of the damaged vessel
congenital: appearing at birth due to a heredity/genetic abnormality or from complications during a pregnancy
connective tissue: the material between the cells of the body that gives tissues form and strength
This tissue is also involved in delivering nutrients.
countercurrent heat exchange: a mechanism used to transfer heat from one flowing current of fluid to another across a semi-permeable membrane
Birds use countercurrent heat exchange between blood vessels in their legs to keep heat concentrated within their bodies.
dehydration: a relative deficiency of water molecules in relation to other dissolved solutes; can be caused by blood loss, vomiting, excess exertion, or malnutrition
diabetes insipidus: a condition characterized by the excretion of large amounts of severely diluted urine, which cannot be reduced when fluid intake is reduced
It denotes an inability of the kidney to concentrate urine. DI is caused by a deficiency of antidiuretic hormone (ADH), also known as vasopressin.
diastole: the relaxation of the heart
distal tubule: the tubular portion of the nephron that lies between the loop of Henle and the proximal tubule
The distal tubule’s main function is the reabsorption of water and solutes and the secretion of various substances.
endocardium: the innermost layer of tissue that lines the chambers of the heart
This sheet of shiny white tissue also lines the body’s blood vessels to help form a continuous lining through the circulatory system. This lining helps blood flow smoothly and prevents the formation of clots.
fibrin: a mesh-like protein involved in the clotting of blood
glomerulus: a fine network of capillaries within Bowman’s capsule arising from the renal artery
helper T-cell: arises from the thymus
These T-cells recognize an antigen on the surface of an invading pathogen and stimulate B-cells to produce antibodies.
hydrostatic pressure: the pressure exerted by a fluid on any contacting surface, such as the force exerted by blood on a capillary wall
Hydrostatic pressure is greater on the arteriole end of a capillary.
hypothalamus: a gland located above the brain stem and connects the nervous system with the endocrine system by relaying messages to the pituitary gland; it is the size of an almond
kidneys: two organs that filter wastes from the blood and adjust the concentration of salts in the blood
The waste is excreted in the urine.
killer T-cell: also known as a cytotoxic T-cell
It kills other target cells, such as cells infected with viruses, parasites, or cancer. These T-cells monitor all the cells of the body and are ready to destroy any cells that express foreign antigen fragments on the surface.
loop of Henle: a tubular portion of the nephron
It is an extension of the proximal tubule that loops into the medulla of the kidney and its main function is the reabsorption of water and ions.
memory T-cell: a lymphocyte that carries receptors for a specific foreign antigen encountered in an earlier infection or through vaccination; it quickly promotes an immune response if the same antigen is re-encountered in a subsequent infection
mitral stenosis: a heart valve disorder that narrows or obstructs the mitral valve opening
Narrowing the mitral valve prevents the valve from opening properly and obstructs the blood flow from the left atrium to the left ventricle. This can reduce the amount of blood that flows forward to the body.
myocardial fibres: a specialized cardiac muscle that can contract as well as conduct electrical impulses; not found anywhere else in the body
osmoreceptors: a sensor found in the hypothalamus of the brain that detects changes in osmotic pressure
osmotic pressure: hydrostatic pressure produced by a solution that is separated by a semi-permeable membrane
The pressure is created due to different concentrations of solutes. It is required to maintain equilibrium with no net movement of solvent. In other words, osmotic pressure stays the same at all times unless there is a problem. You can think of osmotic pressure as the pressure required to prevent water from leaving.
pathogen: a germ or foreign-invading substance that can cause illness/disease
proximal tubule: the tubule connected to Bowman’s capsule
Its main function is the reabsorption of water and solutes as well as the secretion of hydrogen ions.
pulmonary: having to do with the lungs
Purkinje fibres: specialized fibres that transmit electrical impulses to the cardiac muscles in the heart to induce rhythmic muscle contraction
Rh factor: a group of antigens found in most red blood cells; people with Rh antigen on their blood cells are Rh+
shock: a serious, life-threatening condition where insufficient blood flow reaches the body tissues
As the blood carries nutrients and oxygen around the body, reduced flow hinders the delivery of these components to the tissues, and can stop the tissues from functioning properly.
sphygmomanometer: a device used to measure blood pressure
stem cells: undifferentiated cells that can theoretically divide without limit to replenish other cells
When a stem cell divides, each new cell has the potential to either remain a stem cell or become another type of cell with a more specialized function. This can be, for example, a muscle cell, a red blood cell, or a brain cell.
stethoscope: an acoustic medical device designed to listen to internal sounds of the human body
suppressor T-cell: slows and suppresses the process of cellular immunity to ensure that normal tissue does not get destroyed
systemic: a body system in general
systole: a contraction of the heart
undifferentiated cells: not yet reaching the stage where specific biological roles are formed
These cells show no visible separation into their different structural parts.
ureter: in mammals, a pair of muscular tubes that carry urine from the kidneys to the bladder
urethra: the tube through which urine exits the bladder and the body
vasoconstriction: the constriction of blood vessels resulting from muscular contraction in blood vessel walls
When blood vessels constrict, the flow of blood is restricted or slowed. It is the opposite of vasodilation, the widening of blood vessels.