Lesson 1: Clinical Disorders – Part D
| Site: | MoodleHUB.ca 🍁 |
| Course: | Abnormal Psychology 35 RVS |
| Book: | Lesson 1: Clinical Disorders – Part D |
| Printed by: | Guest user |
| Date: | Thursday, 30 October 2025, 1:14 AM |
Section/Lesson Objectives
The student will ...
• Understand and describe the general symptoms of the clinical disorders discussed in the course [This lesson]
• Discuss the possible causes of clinical disorders [This lesson]
• Understand and describe the general symptoms of the cognitive disorders discussed in the course
• Discuss the possible causes of cognitive disorders
• Understand and describe the general symptoms of mental retardation
• Discuss the possible causes of mental retardation
• Understand and describe the general symptoms of the personality disorders discussed in the course
• Discuss the possible causes of personality disorders
Introduction
In the lesson content you will come across some terms in maroon color that are bolded. Look them up in the course Glossary.
Sleeping Disorders
Abnormal sleep is often a contributing factor to many health problems (e.g., heart disease, stroke, high blood pressure). In addition to the physical problems that poor sleep causes, the failure to achieve regular and/or normal sleep can deprive individuals of the joy of life. Lack of sleep reduces alertness, impairs judgement, and affects mood. Impairment to alertness and judgement not only leads to loss of productivity at school or work, but it also contributes to increased accident rates (National Institute of Health, 2004).
 The more than 80 different sleep disorders can be grouped into four main categories:
The more than 80 different sleep disorders can be grouped into four main categories:
1. Problems with falling asleep and staying asleep
2. Problems with staying awake
3. Problems with following a regular sleep schedule
4. Sleep-disruptive behaviours
PART D
Sleep Hygiene
Video: Sleep Hygiene
 Poor sleep habits (referred to as poor sleep hygiene) are linked to many of the sleep problems encountered in North America. For example, many people regularly stay up too late and get up too early. Some people use drugs (caffeine, sleep aids) to force wakefulness or sleep while others over-stimulate themselves with late-night activities such as television.
Poor sleep habits (referred to as poor sleep hygiene) are linked to many of the sleep problems encountered in North America. For example, many people regularly stay up too late and get up too early. Some people use drugs (caffeine, sleep aids) to force wakefulness or sleep while others over-stimulate themselves with late-night activities such as television.
A change in the teenage brain that occurs after puberty, causes sleep patterns to be modified. Teens need around 9 hours of sleep, but studies have found that as many as two thirds of teens get less than seven hours of sleep as changes in their circadian rhythm push them toward later sleep times and most high schools start quite early. A lack of sleep can make a teen prone to depression, being over weight, and hurt their grades along with their athletic performance.
The following information on sleep hygiene, used with permission of the author (University of Iowa and Virtual Hospital, www. vh.org), states that bringing sleep patterns under control and working at a consistent, stable pattern is very important to illness management. We need our rest.
PART D
Do and Don’t
|
DO - Go to bed at the same time each day. DON'T - Engage in stimulating activity just before bed, such as playing a competitive |
 If you lie in bed awake for more than 20-30 minutes, get up, go to a different room (or different part of the bedroom), participate in a quiet activity (e.g., non-excitable reading or television), then return to bed when you feel sleepy. Do this as many times during the night as needed. The most common cause of sleep difficulties relates to changes in a person’s daily routine. For example, travelling, a change in work hours, a disruption of other behaviours (eating, exercise, leisure, etc.), and relationship conflicts may cause sleep problems. Paying attention to good sleep hygiene is the most important thing you can do to maintain quality sleep.
If you lie in bed awake for more than 20-30 minutes, get up, go to a different room (or different part of the bedroom), participate in a quiet activity (e.g., non-excitable reading or television), then return to bed when you feel sleepy. Do this as many times during the night as needed. The most common cause of sleep difficulties relates to changes in a person’s daily routine. For example, travelling, a change in work hours, a disruption of other behaviours (eating, exercise, leisure, etc.), and relationship conflicts may cause sleep problems. Paying attention to good sleep hygiene is the most important thing you can do to maintain quality sleep.
The following general information regarding sleep has been reprinted, with permission, from the National Center on Sleep Disorders Research. Further information can be obtained from their web site.
Sleep is a behavioural state that is a natural part of every individual’s life. We spend about one-third of our lives asleep. Nonetheless, people generally know little about the importance of this essential activity. Sleep is not just something to fill time when a person is inactive. Sleep is a required activity, not an option. Even though the precise functions of sleep remain a mystery, sleep is important for normal motor and cognitive function. We all recognize and feel the need to sleep. After sleeping, we recognize changes have occurred, as we feel rested and more alert. Sleep actually appears to be required for survival. Rats deprived of sleep will die within two to three weeks, a time frame similar to death due to starvation.
A study published in 2009 followed more than 800 patients for three years. They found that of the sleep symptoms, difficulty falling asleep, unrefreshing sleep and loud snoring significantly predicted the development of a metabolic syndrome. This is a condition often marked by obesity, which greatly increases the risk of developing heart disease and diabetes. Therefore getting enough sleep might be part of a good health and weight loss plan.
Problem sleepiness can be deadly. Approximately 100,000 automobile crashes each year result from drivers who were “asleep at the wheel.” In a survey of drivers in New York State, approximately 25 percent reported they had fallen asleep at the wheel at some time. Crashes in which the driver falls asleep are especially common among young male drivers. One large study found that in over 50 percent of fall-asleep crashes, the driver was 25 years old or younger. In addition to the high risk of automobile crashes, problem sleepiness can cause difficulty with learning, memory, thinking, and feeling. These difficulties may lead to poor work performance, and problems with relationships. Furthermore, problem sleepiness leads to errors and accidents in the workplace.
 A study done by Pierre Brochu at the University of Ottawa in 2011, found sleep time decreases when the economy is doing relatively better. When Canadians are in a recession, we get an extra 22 minutes on average per day. This may help explain why there is an increase in accidents seen in boom times. There are increased motor vehicle accidents following both weekends involved with the one-hour daylight time changes. Another study found that adolescents who slept six hours or less were at an increases risk of automobile accidents.
A study done by Pierre Brochu at the University of Ottawa in 2011, found sleep time decreases when the economy is doing relatively better. When Canadians are in a recession, we get an extra 22 minutes on average per day. This may help explain why there is an increase in accidents seen in boom times. There are increased motor vehicle accidents following both weekends involved with the one-hour daylight time changes. Another study found that adolescents who slept six hours or less were at an increases risk of automobile accidents.
The National Highway Traffic Safety Administration has estimated that each year about 100,000 motor vehicle crashes result from drowsy driving.
 |
Teen Mental Health Written by Dr. Stan Kutcher |
PART D
Sleep is a Dynamic Process
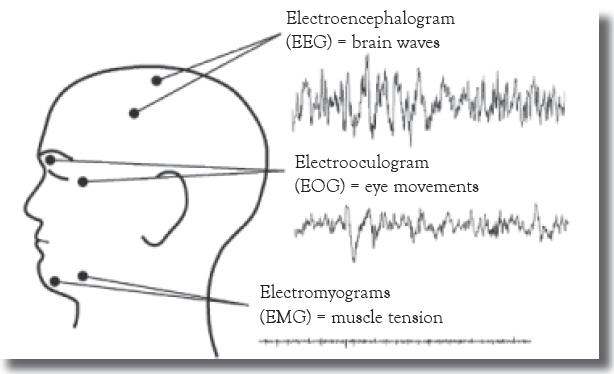
Sleep is not a passive event, but rather an active process involving characteristic physiological changes in the organs of the body. Scientists study sleep by measuring the electrical changes in the brain using electroencephalograms (EEGs). Typically, electrodes are placed on the scalp in a symmetrical pattern. The electrodes measure very small voltages that scientists think are caused by synchronized activity in very large numbers of synapses (nerve connections) in the brain’s outer layers (cerebral cortex). EEG data are represented by curves that are classified according to their frequencies. The wavy lines of the EEG are called brain waves. An electrooculogram (EOG) uses electrodes on the skin near the eye to measure changes in voltage as the eye rotates in its socket. Scientists also measure the electrical activity associated with active muscles by using electromyograms (EMGs). In this technique, electrodes are placed on the skin overlaying a muscle. In humans, the electrodes are placed under the chin because muscles in this area demonstrate very dramatic changes during the various stages of sleep.
In practice, EEGs, EOGs, and EMGs are recorded simultaneously on continuously moving chart paper or digitized by a computer and displayed on a high-resolution monitor.
This allows the relationships among the three measurements to be seen immediately. The patterns of activity in these three systems provide the basis for classifying the different types of sleep.
Figure 3.1:
Placement of electrodes to determine EEG, EOG, and EMG
Studying these events has led to the identification of two basic stages, or states, of sleep: non–rapid eye movement (NREM) and rapid eye movement (REM). Sleep is a highly organized sequence of events that follows a regular, cyclic program each night. Thus, the EEG, EMG, and EOG patterns change in predictable ways several times during a single sleep period. NREM sleep is divided into four stages according to the amplitude and frequency of brain wave activity. In general, the EEG pattern of NREM sleep is slower, often more regular, and usually of higher voltage than wakefulness. As sleep gets deeper, the brain waves get slower and have greater amplitude. NREM Stage 1 is very light sleep; NREM Stage 2 has special brain waves called sleep spindles and K complexes; NREM Stages 3 and 4 show increasingly more high-voltage slow waves. In NREM Stage 4, it is extremely difficult to be awakened by external stimuli. The muscle activity of NREM sleep is low, but the muscles retain their ability to function. Eye movements normally do not occur during NREM sleep, except for very slow eye movements, usually at the beginning. The body’s general physiology during these stages is fairly similar to the wake state.
Figure 3.2: Characteristic EEG, EOG, and EMG patterns for wakefulness, REM sleep, and NREM sleep. Each of the nine patterns was made over a period of about three seconds [a three-second sample].
Figure 3.2:
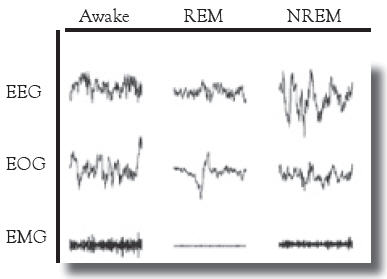
The EEG recorded during REM sleep shows very fast and desynchronized activity that is more random than that recorded during NREM sleep. It actually looks similar to the EEG (low voltage with a faster mix of frequencies) from when we are awake. REM sleep is characterized by bursts of rapid eye movements. The eyes are not constantly moving, but they dart back and forth or up and down. They also stop for a while and then jerk back and forth again. Always, and just like waking eye movements, both eyes move together in the same direction. Some scientists believe that the eye movements of REM sleep relate to the visual images of dreams, but why they exist and what function they serve, if any, remain unknown. Additionally, while muscle tone is normal in NREM sleep, we are almost completely paralyzed in REM sleep. Although the muscles that move our bodies go limp, other important muscles continue to function in REM sleep. These include the heart, diaphragm, eye muscles, and smooth muscles such as those of the intestines and blood vessels. The paralysis of muscles in the arms and legs and under the chin show electrical silence in REM sleep. On an EMG, the recording produces a flat line. Small twitches can break through this paralysis and look like tiny blips on the flat line.
PART D
Sleep is a Cyclical Process
During sleep, people experience repeated cycles of NREM and REM sleep, beginning with an NREM phase. This cycle lasts approximately 90 to 110 minutes and is repeated four to six times per night. As the night progresses, however, the amount of deep NREM sleep decreases and the amount of REM sleep increases. The term ultradian rhythm (that is, rhythm occurring within a period of less than 24 hours) is used to describe this cycling through sleep stages.
PART D
Sleep Patterns
Sleep patterns change during an individual’s life. In fact, age affects sleep more than any other natural factor. Newborns sleep an average of 16 to 18 hours per day. By the time a child is three to five years old, total sleep time averages 10 to 12 hours, and then it further decreases to 7 to 8 hours per night by adulthood. One of the most prominent age-related changes in sleep is a reduction in the time spent in the deepest stages of NREM (Stages 3 and 4) from childhood through adulthood. In fact, this change is prominent during adolescence, when about 40 percent of this activity is lost and replaced by Stage 2 NREM sleep. In addition to these changes, the percentage of time spent in REM sleep also changes during development. Newborns may spend about 50 percent of their total sleep time in REM sleep. In fact, unlike older children and adults, infants fall asleep directly into REM sleep. Infant sleep cycles generally last only 50 to 60 minutes. By two years of age, REM sleep accounts for 20 to 25 percent of total sleep time, which remains relatively constant throughout the remainder of life. Young children have a high arousal threshold, which means they can sleep through loud noises, especially in the early part of the night. For example, one study showed that 10-year-olds were undisturbed by a noise as loud as the sound of a jet airplane taking off nearby.
Although most humans maintain REM sleep throughout life, brain disorders such as Alzheimer’s and Parkinson’s are characterized by decreasing amounts of REM sleep as the diseases progress. Also, elderly individuals exhibit more variation in the duration and quality of sleep than do younger adults. Elderly people may also exhibit increased sleep fragmentation (arousals from sleep that occur as either short or more extended awakenings). Overall, several issues are important to consider. First, individual sleep needs vary. For instance, eight hours of sleep per night appears to be optimal for most adults although some may need more or less. Teenagers, on average, require about nine or more hours of sleep per night to be as alert as possible when awake. If sleep needs are not met, a progressive sleep debt occurs, and eventually the body requires that the debt be paid. We seem unable to adapt to getting less sleep than our bodies require. Not getting enough sleep, while still allowing us to function in a seemingly normal manner, does impair motor and cognitive functions. Caffeine and other stimulants cannot substitute for sleep, but they do help to counteract some of the effects of sleep deprivation.
Video: Teenage Sleep
PART D
Biological Clocks
An internal biological clock regulates the timing for sleep in humans. The activity of this clock makes us sleepy at night and awake during the day. Our clock cycles with an approximately 24-hour period and is called a circadian clock. In humans, this clock is located in the suprachiasmatic nucleus (SCN) of the hypothalamus in the brain (see Figure 6.1). The SCN is actually a very small structure consisting of a pair of pinhead-size regions, each containing only about 10,000 neurons of the brain’s estimated 100 billion neurons.
Figure 6.1
The biological clock is located within the suprachiasmatic nucleus in the brain.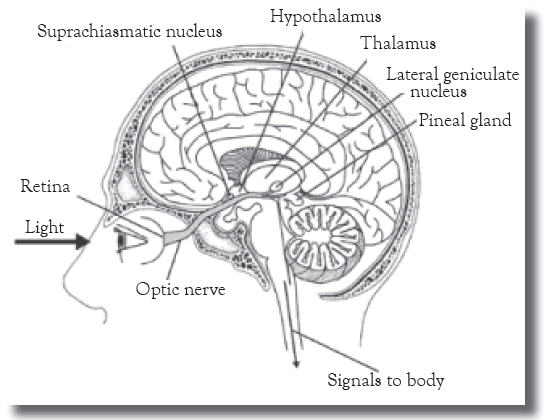
Biological clocks are genetically-programmed physiological systems that allow organisms to live in harmony with natural rhythms, such as day/night cycles and the changing of seasons. The most important function of a biological clock is to regulate overt biological rhythms such as the sleep/wake cycle. The biological clock is also involved in controlling seasonal reproductive cycles in some animals through its ability to track information about the changing lengths of daylight and darkness during a year.
Biological rhythms are of two general types. Exogenous rhythms are directly produced by an external influence, such as an environmental cue. They are not generated internally by the organism itself, and if the environmental cues are removed, the rhythm ceases. Endogenous rhythms, by contrast, are driven by an internal, self-sustaining biological clock rather than by anything external to the organism. Biological rhythms, such as oscillations in core body temperature, are endogenous. They are maintained even if environmental cues are removed.
Because the circadian clock in most humans has a natural day length of just over 24 hours, the clock must be entrained, or reset, to match the day length of the environmental photoperiod (that is, the light/dark, or day/night, cycle). The cue that synchronizes the internal biological clock to the environmental cycle is light. Photoreceptors in the retina transmit light-dependent signals to the SCN. Interestingly, our usual visual system receptors, the rods and cones, are apparently not required for this photoreception. Special types of retinal ganglion cells are photoreceptive, project directly to the SCN, and appear to have all the properties required to provide the light signals for synchronizing the biological clock. At the SCN, the signal interacts with several genes that serve as “pacemakers.”
Figure 6.2:
Body temperature in relation to the sleep cycle
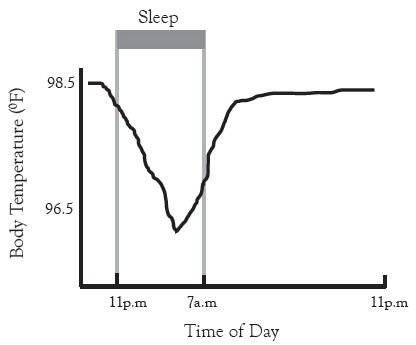
Another interesting rhythm that is controlled by the biological clock is the cycle of body temperature, which is lowest in the biological night and rises in the biological daytime. This fluctuation persists even in the absence of sleep. Activity during the day and sleep during the night reinforce this cycle of changes in body temperature, as seen in Figure 6.2.
The release of melatonin, a hormone produced by the pineal gland, is controlled by the circadian clock in the SCN. Its levels rise during the night and decline at dawn in both nocturnal and diurnal species. (Nocturnal animals are more active at night and diurnal animals are more active during the day). Melatonin has been called the hormone of darkness because of this pattern. The SCN controls the timing of melatonin release; melatonin then feeds back on the SCN to regulate its activity. In mammals, for example, most of the brain receptors for melatonin are located in the SCN. Research has demonstrated that administering melatonin can produce shifts in circadian rhythms in a number of species including rats, sheep, lizards, birds, and humans. These effects are most clearly evident when melatonin is given in the absence of light input. For example, giving melatonin to blind people can help set their biological clocks. Melatonin is available as an over-the-counter nutritional supplement. Although claims are made that the supplement promotes sleep, the evidence for this is inconclusive. Potential side effects of long-term administration of melatonin remain unknown, and its unsupervised use by the general public is discouraged.
In addition to synchronizing these daily rhythms, biological clocks can affect rhythms that are longer than 24 hours, especially seasonal rhythms. Some vertebrates have reproductive systems that are sensitive to day length. These animals can sense changes in day length by the amount of melatonin secreted. The short days and long nights of winter turn off the reproductive systems of hamsters while in sheep the opposite occurs. The high levels of melatonin that inhibit reproduction in hamsters stimulate the reproductive systems of sheep, so they breed in winter and give birth in the spring.
One negative consequence of our circadian cycle afflicts travellers who rapidly cross multiple time zones. Jet lag produces a number of unwanted effects including excessive sleepiness, poor sleep, loss of concentration, poor motor control, slowed reflexes, nausea, and irritability. Jet lag results from the inability of our circadian clock to make an immediate adjustment to the changes in light cues that an individual experiences when rapidly crossing time zones. After such travel, the body is in conflict. The biological clock carries the rhythm entrained by the original time zone although the clock is out of step with the cues in the new time zone. This conflict between external and internal clocks and signals is called desynchronization, and it affects more than just the sleep/wake cycle. All the rhythms are out of sync, and they take a number of days to re-entrain to the new time zone.
Eastward travel generally causes more severe jet lag than westward travel, because traveling east requires that we shorten our day and adjust to time cues occurring earlier than our clock is used to.
In general, the human circadian clock appears better able to adjust to a longer day than a shorter day. For example, it is easier for most people to adjust to the end of daylight savings time in the fall when we have one 25-hour day than to the start of daylight savings time in the spring, when we have a 23-hour day. Similarly, traveling from the West Coast to the East Coast produces a loss of three hours—a 21-hour day. Thus, travellers may find sleeping difficult because of the three-hour difference between external cues and their internal clocks. Likewise, travelers may find awakening difficult in the morning. We may try to go to sleep and wake up at our usual local times of, say, 11 p.m. and 7 a.m., but to our brain’s biological clock, the times are 8 p.m. and 4 a.m
Other circadian rhythm problems include the following:
|
1. Monday morning blues. By staying up and sleeping an hour or more later than usual on the weekends, we provide our biological clock different cues that push it toward a later nighttime phase. By keeping a late sleep schedule both weekend nights, our internal clock becomes two hours or more behind our usual weekday schedule. When the alarm rings at 6:30 a.m. on Monday, our body’s internal clock is now set for 4:30 a.m. or earlier. 2. Seasonal affective disorder (SAD). A change of seasons in autumn brings on both a loss of daylight savings time (fall back one hour) and a shortening of the daytime. As winter progresses, the day length becomes even shorter. During this season of short days and long nights, some individuals develop symptoms similar to jet lag but more severe. These symptoms include decreased appetite, loss of concentration and focus, lack of energy, feelings of depression and despair, and excessive sleepiness. Too little bright light reaching the biological clock in the SCN appears to bring on this recognized form of depression in susceptible individuals. Consequently, treatment often involves using light therapy. 3. Shift work. Unlike some animals, humans are active during daylight hours. This pattern is called diurnal activity. Animals that are awake and active at night (for example, hamsters) have what is known as nocturnal activity. For humans and other diurnally active animals, light signals the time to awake, and sleep occurs during the dark. Modern society, however, requires that services and businesses be available 24 hours a day, so some individuals must work the night shift. These individuals no longer have synchrony between their internal clocks and signals of external daylight and darkness. They may experience mental and physical difficulties similar to jet lag and SAD. |
PART D
Functions of Sleep
Animal studies have demonstrated that sleep is essential for survival. Laboratory rats will normally live for two to three years; rats deprived of REM sleep survive an average of only five months. Rats deprived of all sleep survive only about three weeks. In humans, extreme sleep deprivation can cause an apparent state of paranoia and hallucinations in otherwise healthy individuals. However, despite identifying several physiological changes that occur in the brain and body during sleep, scientists still do not fully understand the functions of sleep.
Sleep also allows the brain to be cleansed by cerebral spinal fluid. Since we do not have lymph vessels in the brain to remove waste, the brain has a unique way of cleansing itself when we sleep. Please watch the video below.
Video: One more reason to get a good night's sleep
Benefits of Sleep
Athletics - There is a link between insufficient sleep and reaction time. A lack of sleep can lead to  completely missed cues (eg. you don't see the pitcher releasing the baseball) and a slowed reaction time (you see the pitch but react too slowly. A study published in 2011 looked at the Stanford men's varsity basketball team. The students were told to get as much sleep as possible. They had no trouble complying and got an average of 111 minutes of extra sleep. After two to four weeks of this, they were not only better athletes, they were happier. The subjects also reported improved overall ratings of physical and mental well-being during practices and games. A similar study involving swimmers found more sleep time brought faster times in the pool. Athletes from all sports can benefit from extra sleep time in order to get the additional competitive edge to perform at their highest level.
completely missed cues (eg. you don't see the pitcher releasing the baseball) and a slowed reaction time (you see the pitch but react too slowly. A study published in 2011 looked at the Stanford men's varsity basketball team. The students were told to get as much sleep as possible. They had no trouble complying and got an average of 111 minutes of extra sleep. After two to four weeks of this, they were not only better athletes, they were happier. The subjects also reported improved overall ratings of physical and mental well-being during practices and games. A similar study involving swimmers found more sleep time brought faster times in the pool. Athletes from all sports can benefit from extra sleep time in order to get the additional competitive edge to perform at their highest level.
Learning - Although we gather information while we are awake, we learn it while we are sleeping. The brain restores the synapses, taking the information worth keeping and learning it. The brain also flushes out the useless information that we do not use.
Healthy Bodies - There is a link between lack of sleep and weight gain. Fat is not metabolized very well at night, resulting in lipid levels and blood glucose. The body does not process and store nutrients at night as it does during the day. Skin can suffer too. You look better after a good nights sleep. Studies also link lack of sleep and illness in teens. Males in particular are more likely to get a cold when they lack sleep.
Improves mental outlook: Depression and sleep issues have been linked in many studies, including a 2008 report that tied sleep disturbances to suicide in teens.
Reference: Gabriella Boston, The Washington Post

PART D
Specific Sleep Disorders
Problems with sleep can be due to lifestyle choices and can result in problem sleepiness—that is, feeling sleepy at inappropriate times. Environmental noise, temperature changes, changes in sleeping surroundings, and other factors may affect our ability to get sufficient restful sleep. Short-term problem sleepiness may be corrected by getting additional sleep to overcome the sleep deficit. In other cases, problem sleepiness may indicate a sleep disorder requiring medical intervention. Alcohol abuse can cause or exacerbate sleep disorders by disrupting the sequence and duration of sleep states. Alcohol does not promote good sleep, and consuming alcohol in the evening can also exacerbate sleep apnea problems.
Insomnia, the most prevalent sleep disorder, is characterized by an inability to fall asleep and/or by waking up during the night and having difficulty going back to sleep. Primary insomnia is more common in women than men and tends to increase with age. Short-term or transient insomnia may be caused by emotional or physical discomfort, stress, environmental noise, extreme temperatures, or jet lag. Transient insomnia may also result as a side effect of medication. Secondary insomnia may result from a combination of physical or mental disorders, undiagnosed or uncontrolled sleep disorders (that is, sleep apnea, restless legs syndrome, narcolepsy, and circadian rhythm disorders), and effects of prescription or non-prescription medications. Treatment differs for primary and secondary causes of insomnia. Treatment may include following a specific night-time routine, improving one’s sleep environment, reducing caffeine and alcohol intake, or reducing afternoon napping. Pharmacological treatments may alleviate symptoms in specific cases. Some individuals try to overcome the problem of insomnia by drinking alcoholic beverages. Alcohol inhibits REM sleep and the deeper, restorative stages of sleep, and, therefore, does not promote restful sleep.

Obstructive sleep apnea (OSA) is a potentially life-threatening disorder in which breathing is interrupted during sleep. Over 12 million North Americans have OSA. This condition may be associated with bony or soft tissue that limits airway dimensions and is made worse in the presence of excess fatty tissue. Repetitive episodes of no effective breath, very shallow breaths, or adequate breaths but with high airway resistance can occur 20 to 30 times per hour or more. These episodes cause temporary drops in blood oxygen and increases in carbon dioxide levels, which lead to frequent partial arousals from sleep. Limitations in upper-airway dimensions are typically associated with chronic loud snoring. The frequent arousals result in ineffective sleep and account for the chronic sleep deprivation and the resultant excessive daytime sleepiness that is a major hallmark of this condition. Additional effects include morning headaches, high blood pressure, heart attacks, heart-rhythm disorders, stroke, and decreased life expectancy. OSA also occurs in children and is generally related to enlarged tonsils or adenoids. It occurs equally often in boys and girls and is most common in preschool-age children.
Because many of the factors contributing to OSA appear to have significant genetic influences (such as bony dimensions of upper airways), genetic risk factors are likely important in the occurrence of OSA. Treatment for adult OSA can include behavioral therapy (losing weight, changing sleeping positions, and avoiding alcohol, tobacco, and sleeping pills), use of mechanical devices (continuous positive airway pressure to force air through the nasal passages, or dental appliances that reposition the lower jaw and tongue), and surgery to increase the size of the airway.
Restless legs syndrome (RLS) is a neurologic movement disorder that is often associated with a sleep complaint. People with RLS have unpleasant leg sensations and an almost irresistible urge to move the legs. Symptoms are worse during inactivity and often interfere with sleep. RLS sufferers report experiencing creeping, crawling, pulling, or tingling sensations in the legs (or sometimes the arms) that are relieved by moving or rubbing them. Sitting still for long periods becomes difficult; symptoms are usually worse in the evening and night and less severe in the morning. Periodic leg movements, which often coexist with restless legs syndrome, are characterized by repetitive, stereotyped limb movements during sleep. Periodic limb movement disorder can be detected by monitoring patients during sleep. Some people with mild cases of RLS can be treated by exercise, leg massages, and eliminating alcohol and caffeine from the diet. Others require pharmacological treatment, and to determine the right medication or combination of medications for the individual may take time. Estimates suggest that RLS may affect between 10 and 15 percent of the population.
Video: Restless Leg Syndrome
Narcolepsy is a chronic sleep disorder that usually becomes evident during adolescence or young adulthood and can affect both men and women. In the United States, it affects as many as 250,000 people although fewer than half are diagnosed. The main characteristic of narcolepsy is excessive and overwhelming daytime sleepiness (even after adequate nighttime sleep). A person with narcolepsy is likely to become drowsy or to fall asleep at inappropriate times and places. Daytime sleep attacks may occur with or without warning and may be irresistible. In addition, nighttime sleep may also be fragmented. Three other classic symptoms, which may not occur in all people with narcolepsy, are cataplexy (sudden muscle weakness often triggered by emotions such as anger, surprise, laughter, and exhilaration), sleep paralysis (temporary inability to talk or move when falling asleep or waking up), and hypnagogic hallucinations (dreamlike experiences that occur while dozing or falling asleep).
People with narcolepsy have difficulty staying awake, and in extreme conditions, narcoleptic episodes can occur during periods of activity. Narcolepsy is not the same as simply becoming tired or dozing in front of the TV after a day’s work.
REM sleep in people with narcolepsy frequently occurs at sleep onset instead of after a period of NREM sleep. Consequently, researchers believe that the symptoms of narcolepsy result from a malfunction in some aspect of REM sleep initiation. Some scientists believe that the immune system causes narcolepsy by attacking the nervous system (that is, an autoimmune response). In this view, exposure to an unknown environmental factor results in an immune response against nerve cells in the brain circuits that control arousal and muscle tone. The discovery of a narcolepsy gene in dogs indicates that genetic risk factors for narcolepsy may also be pertinent in humans. Studies of narcoleptic dogs suggest that altered receptors for a specific neurotransmitter in the hypothalamus can cause cataplexy and the other symptoms of narcolepsy. Many individuals with narcolepsy appear to have a deficiency of this hypothalamic transmitter. Although no definitive cure for narcolepsy, is available several treatment options alleviate various symptoms. Treatment is individualized depending on the severity of the symptoms, and it may take weeks or months for the optimal regimen to be determined. Treatment is primarily by medications, but lifestyle changes are also important.
Video: What is Narcolepsy?
 Parasomnias are sleep disorders that involve a range of behaviors that occur during sleep. These include sleepwalking, sleep talking, enuresis (bed-wetting), and sleep terrors, which are NREM disorders that occur early in the night. Many of the parasomnias (including sleepwalking, sleep talking, and sleep terrors) are more common in children. Children generally have no memory of such events, usually do not require treatment, and usually outgrow the disorder. Enuresis may respond to drug treatment, and like other parasomnias in children, it generally resolves as the child becomes older.
Parasomnias are sleep disorders that involve a range of behaviors that occur during sleep. These include sleepwalking, sleep talking, enuresis (bed-wetting), and sleep terrors, which are NREM disorders that occur early in the night. Many of the parasomnias (including sleepwalking, sleep talking, and sleep terrors) are more common in children. Children generally have no memory of such events, usually do not require treatment, and usually outgrow the disorder. Enuresis may respond to drug treatment, and like other parasomnias in children, it generally resolves as the child becomes older.
REM sleep behavior disorder is a parasomnia that occurs later in the night than NREM disorders. It differs from the parasomnias discussed previously because it usually affects middle-aged or elderly individuals. Frequently, sufferers will also have a neurological disorder. The temporary muscle paralysis that normally occurs during REM sleep does not occur in this disorder. Because the muscles are not paralyzed, individuals may act out potentially violent behaviors during sleep and cause injuries to themselves or their bed partners.
PART D
Kleine-Levin Syndrome - An Uncommon Sleep Disorder
Kleine-Levin syndrome is a rare disorder that results in recurring episodes of excessive drowsiness and sleep (up to 20 hours per day). Symptoms that may last for days to weeks include an increase in appetite, irritability, confusion, lack of energy, and hypersensitivity to noise. Some people may experience hallucinations and have an unconstrained sex drive. Affected individuals function normally between occurrences, but brief periods of depression and amnesia may occur after an episode.
Periods of multiple weeks between episodes are common with the typical age of initial onset occurring between adolescence and late teen years. Fortunately, the symptoms of Kleine-Levin syndrome improve markedly or disappear completely over time. This sleep disorder is four times more common in males than in females, and symptoms may be related to malfunction of the hypothalamus, the part of the brain that governs appetite and sleep. The disorder appears to be benign (not harmful) and does not significantly impact psychological or physical functioning of afflicted individuals.
Lesson Review
Lesson 1 Part D is all about sleep, did you succomb to sleep while reading the course material
|
To summarize: • Sleep Hygiene • Do and Don’t • Sleep is a Dynamic Process • Sleep is a Cyclical Process • Sleep Patterns • Biological Clocks • Functions of Sleep • Specific Sleep Disorders • Kleine-Levin Syndrome - An Uncommon Sleep Disorder |
Assignment
Complete S3L1C_DQuiz. You may refer to your lesson while you complete this quiz.
 evidence that regular exercise improves restful sleep. This includes stretching and aerobic exercise.
evidence that regular exercise improves restful sleep. This includes stretching and aerobic exercise.  drowsiness.
drowsiness.  game, watching an exciting television program or movie, or having an important discussion with a loved one.
game, watching an exciting television program or movie, or having an important discussion with a loved one. 