Module 4
| Site: | MoodleHUB.ca 🍁 |
| Course: | Biology 30 SS |
| Book: | Module 4 |
| Printed by: | Guest user |
| Date: | Friday, 19 December 2025, 4:08 AM |
Description
Created by IMSreader
1. Module 4
Module 4—From Fertilization to Birth
Introduction
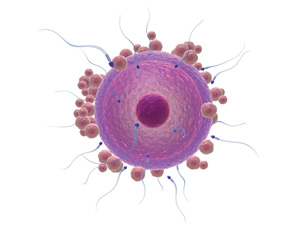
When the sperm from your father met the egg from your mother, your genetic features were established through the union of two parental sets of deoxyribonucleic acid (DNA). DNA also directed the unicellular fertilized egg through cell divisions to become a multicellular organism. During this developmental period, cells responded to DNA by differentiating and specializing into the tissues, organs, and systems that make up your body. Hormones regulated this development. In addition to genetic factors dictating, and hormonal factors regulating, your prenatal development, environmental factors also affected your development.
In this module you will come to understand the process of gestation. You will examine what happens to the egg after it has been fertilized, the developmental stages of the embryo and fetus, and finally how the birthing process produces a new offspring. You will also examine how reproductive technologies can enhance fertilization and how they are used in the birthing process.
1.1. Big Picture
Module 4—From Fertilization to Birth
 Big Picture
Big Picture

© digitalskillet/iStockphoto
Most people love babies. Images of babies are used to sell everything from diapers to cars.
Between conception and birth, a period of approximately 40 weeks, the fertilized egg divides, differentiates, and specializes to form a complex multicellular organism. The fertilized egg begins its journey down the Fallopian tube and undergoes many changes before implanting in the uterus. In the first eight weeks of development and differentiation, many factors can have impacts on the embryo. Many support structures are formed to facilitate the embryo’s development. From fertilization all the way through until birth, different hormones regulate and control the progression of prenatal development. Environmental factors can also affect the developing embryo and fetus. Reproductive technologies can be used to enhance or reduce reproductive potential, but there are often societal issues related to the use of these technologies.
Dividing the prenatal development and parturition events into different periods or stages is a way to gauge normal progress. That being said, it is important to remember that not all development and labour will follow the exact time frames given. These events progress at slightly different rates in each woman and in each individual pregnancy; no two pregnancies are exactly alike. However, it is important that you understand the overall progress and relative time periods described. Many factors and technologies can prevent or assist in prenatal development and observation.
In this module you will continue to help three couples, Jane and John, Olga and Karl, and Maria and José, who have come to you for help with their infertility problems. Throughout the module, further issues will come to light and decisions will need to be made by the couples in order for them to achieve their goal of having children.
Throughout the module you will explore the following focusing questions:
- What are the sequences of events and hormone controls that occur throughout fertilization and embryonic development?
- What major tissues and organs arise from the ectoderm, mesoderm, and endoderm?
- How are twins formed?
- What are the major events of each trimester?
- What is the significance of the first trimester?
- What is the significance of the effects of teratogens on embryonic and fetal development?
- What triggers the birthing process, and what are its stages?
- What controls lactation?
- What technologies are used to assist fertilization, to monitor development, and to facilitate parturition?

© emin kuliyev/shutterstock
You have been introduced to the focusing questions for this module. Each lesson will restate these focusing questions to guide your study. To help you organize the concepts of this module, and to provide you with a potential aid for review, you may choose to download the Module 4 Concept Organizer. Fill in this concept organizer with the ideas that you master as you work through each lesson, or prepare the organizer when you have completed Module 4. You can use keywords, point form, or any amount of detail that meets your needs. You may choose to work from the file on your computer, print the document and work from the paper copy, or copy the outline onto a large sheet of poster paper. After you have prepared your concept organizer, you may wish to check your work with the concept organizer provided in the Module Summary. The concept organizer provided outlines some of the key topics that you should include in each lesson of your concept organizer. This is a great tool to review and use for study purposes, but using this organizer is completely your choice.
The Module Assessment for Module 4 involves completing a table outlining the genetic, hormonal, and environmental effects on embryonic and fetal development.
Throughout Module 4 you will continue to work toward the Unit B Assessment on the fertility case study involving three couples struggling with infertility. You may choose to recall the requirements of the Unit B Assessment by reading “A Fertility Case Study.” Keep in mind what you have discovered about the couples so far from your work in Module 3 and what treatment options you have already provided. Add to your information as you work through Module 4. You will need this information to complete the Unit B Assessment.
1.2. In this Module
Module 4—From Fertilization to Birth
In This Module
Inquiry Question: From fertilization to birth, how is cell differentiation and development regulated by genetic, endocrine, and environmental factors?
There are four lessons in Module 4.
Most of the lessons are designed to take you 80 minutes to complete; however, some lessons may take longer because of the significance of the concept being covered in the lesson. The suggested lesson times do not include the time needed to complete such activities as “Try This,” “Watch and Listen,” assignments, practice questions, review, or research.
This module corresponds to Chapter 15, pages 506 to 543, in your textbook. You may choose to quickly read through these pages for an overview before you begin Module 4.
Module 4 examines the structures, and their functions, and the major events associated with fertilization up to the completion of embryonic development. The characteristics and events associated with fetal development are also examined; from the time directly following embryonic development up to and including birth. Furthermore, the effects of hormones and environmental factors that can have implications for development are also studied. Finally, this module examines the technologies that are available for the enhancement or reduction of reproductive potential.
Lesson 1—Fertilization and Embryonic Development
This lesson describes the process of embryonic development, names the major events, and describes membrane formation that occurs. You will learn to identify the germ layers, state what structures arise from each layer, describe the hormones related to fertilization and pregnancy, and describe how twins are formed.
The following focusing questions are addressed in this lesson:
- What are the sequences of events and hormone controls that occur throughout fertilization and embryonic development?
- What major tissues and organs arise from the ectoderm, mesoderm, and endoderm?
- How are twins formed?
Lesson 2—Fetal Development, Trimester Events, and Environmental Factors
In this lesson you will learn the major events of fetal development related to each of the trimesters and the significance of the first trimester. You will study potentially harmful substances that can cause damage during embryonic and fetal development.
The following focusing questions are addressed in this lesson:
- What are the major events of each trimester?
- What is the significance of the first trimester?
- What is the significance of the effects of teratogens on embryonic and fetal development?
Lesson 3—Hormones and the Birthing Process
In this lesson you will learn to relate the neural and hormonal changes that occur at the end of pregnancy to the physiological effects of the birthing process.
The following focusing questions are addressed in this lesson:
- What triggers the birthing process, and what are its stages?
- What controls lactation?
Lesson 4—Reproductive Technologies—Enhancing or Reducing Fertility, Monitoring Development, and Use in Parturition
In this lesson you will come to understand how technology can be used to enhance or reduce fertility, monitor fetal development, and assist in parturition.
The following focusing question is addressed in this lesson:
- What technologies are used to assist fertilization, to monitor development, and to facilitate parturition?
Module 4 Assessment
Working with a partner or small group that has been approved by your teacher, show your understanding of this module’s content by planning, designing, and creating a multimedia presentation. Make sure you include the following points in your presentation:
- Describe all major events and components of prenatal development, from fertilization to the end of the fetal development period, including hormonal control and significant developmental events happening in each trimester.
- State and describe three factors that affect embryonic and fetal development. These must include one genetic factor, one hormonal factor, and one environmental factor. For each of these three factors, state how the embryonic germ tissue is affected and how this may or may not affect fetal development.
- Examine parturition events and explain the hormonal and neural components that cause the onset of labour and sustain the birthing process through to the end of the placental stage.
- Describe the events that need to happen for successful lactation to occur.
- Examine reproductive technologies and describe at least one technology that enhances reproductive potential, at least one technology that reduces reproductive potential, and at least one technology that is used to monitor embryonic or fetal development. Be sure to discuss any societal, cultural, environmental, ethical, or economic considerations surrounding the use of these technologies.
Rubric
The following rubric will help you prepare your response. Remember that complete, clearly explained work is necessary when responding to this type of question. The points above are worth 5 marks each, making your presentation worth a total of 25 marks.
Score |
Prenatal Development |
Affecting Factors |
Parturition Events |
Lactation |
Reproductive Technologies |
5 |
Clearly identifies all prenatal development, including where the events are occurring. This includes fertilization and implantation. |
Identifies three factors that affect embryonic and fetal development structures—one of each chromosomal, hormonal, and environmental. |
Clearly explains parturition events. |
Fully describes hormonal and neural control of lactation. |
Fully describes each reproductive technology that assists in enhancing reproductive potential, reducing reproductive potential, and monitoring embryonic or fetal development. |
4 |
Clearly identifies most prenatal development and includes where the events are occurring. This includes fertilization and implantation. |
Identifies three factors that affect embryonic and fetal development structures—one of each chromosomal, hormonal, and environmental. |
Clearly explains parturition events. |
Describes hormonal and nerve control of lactation. |
Describes a reproductive technology that assists in enhancing reproductive potential, reducing reproductive potential, and monitoring embryonic or fetal development. |
3 |
Identifies some prenatal development and includes where the events are occurring. This includes fertilization and implantation. |
Identifies two factors that affect embryonic and fetal development structures—two of either chromosomal, hormonal, or environmental. |
Explains some of the parturition events. |
Describes only hormonal, not neural, control of lactation. |
Describes only two of the following—reproductive technologies that assist in enhancing reproductive potential, reducing reproductive potential, and/or monitoring embryonic or fetal development. |
2 |
Lacking much detail of prenatal development, does not include where the events are occurring. |
Identifies two factors that affect embryonic and fetal development structures—two of either chromosomal, hormonal, or environmental. |
Names only the parturition events. |
Describes only some of the hormonal control of lactation, does not describe neural control of lactation. |
Describes only two of the following— reproductive technologies that assist in enhancing reproductive potential, reducing reproductive potential, and/or monitoring embryonic or fetal development. |
1 |
Addresses only one of the bullets at a 2 or 3 level. |
Addresses only one of the bullets at a 2 or 3 level. |
Addresses only one of the bullets at a 2 or 3 level. |
Addresses only one of the bullets at 2 or 3 level. |
Addresses only one of the bullets at a 2 or 3 level. |
1.3. Lesson 1
Module 4—From Fertilization to Birth
Lesson 1—Fertilization and Embryonic Development
 Get Focused
Get Focused
All the structures and functions of mammalian reproductive systems are designed to support the fertilization, implantation, and development of an embryo and, later, fetus. These processes finally result in the continuation of the species through the birth of a new offspring.
fertilization: the fusing of a sperm nucleus with an egg nucleus to form a zygote; occurs in the oviduct
implantation: burrowing of the blastocyst into the wall of the endometrium of the uterus
embryo: the organism in the stages of development from the time the zygote begins cleavage until nine weeks of gestation, when the embryo becomes a fetus
fetus: the organism in the stages of development from nine weeks until birth
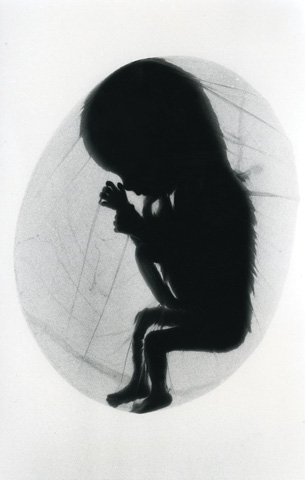
© Sebastian Kaulitzki/Shutterstock
© Jenny Horne/Shutterstock

© shahar choen/Shutterstock
How does an offspring go from being a single-cell zygote, which is totally dependent on its mother during its “internal” life in utero, to an organism made up of billions of cells, which is able to survive independently from its mother? The processes that take place from fertilization through to the maturation of the fetus are astounding, and it all starts with just two cells.
© Christian Darkin/shutterstock
Previous lessons introduced the structures and functions of the male and female reproductive systems. You also learned about the hormones that cause the development and the onset of function of these systems. In this lesson you will study the events that occur at fertilization and throughout the eight-week development of the embryo.
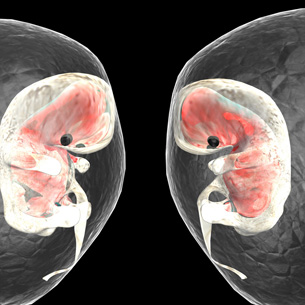
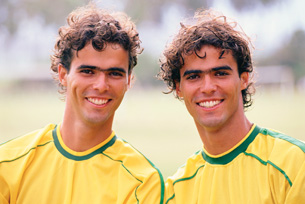
Jane and John, whom you met in your introduction to the Fertility Case Study you will be completing throughout this module, were thrilled when they heard the news that they were going to be parents for the first time. They were still thrilled, but a bit surprised, when they discovered they were going to have twins. Imagine how much more surprised they will be when the twins are born with two different skin colours! The probability of this happening is about 1 million to 1. In this lesson you will discover how the different types of twins form and you will be able to explain how giving birth to twins with different skin colours might be possible.
Whether embryos develop as twins or as a single child, their development in the uterus is the same. An offspring’s embryonic development occurs as a vast array of changes beginning with an egg and a sperm uniting in fertilization to form a new individual. Specific names are given to the different stages of embryonic growth and maturation. It should be noted that these various stages of prenatal development contribute to the hormonal control that sustains the pregnancy.
The prenatal development of an offspring is divided into two developmental periods. The first takes place from fertilization to the end of the eighth week of pregnancy. During this period the developing offspring is called an embryo. The second developmental period takes place from the ninth week of pregnancy to birth. During this period the developing offspring is called a fetus.
extra-embryonic membranes: membranes surrounding the embryo, and later the fetus, that support its development in different ways; include the allantois, amnion, chorion, and yolk sac
In addition to the development of the embryo, there are supporting structures that must be formed at the same time. The supporting structures are collectively called the extra-embryonic membranes and they provide the embryo, and later the fetus, with means of nutrition, respiration, excretion, and protection.
Within the first two months of embryonic development, almost all of the organ systems are formed and the embryo begins to appear humanlike. It’s no wonder pregnant women are often very tired in the first few weeks of their pregnancy! All energy and nutritional requirements for prenatal growth come from the mother’s body.

© Stephen Mcsweeny/Shutterstock

© James Blinn /shutterstock

© Tomasz Trojanowski/Shutterstock
© 2008 Jupiterimages Corporation
dizygotic twins: twins that form when two eggs are fertilized by two sperms; also known as fraternal twins; may be of different sexes
monozygotic twins: identical twins formed when the embryonic mass produced by the union of one egg and one sperm splits into two separate, identical masses; are of the same sex
How did Jane and John’s pregnancy result in the formation of twins? There are two ways in which twins can be formed. In a normal sequence of events, a woman releases one egg every menstrual cycle. However, it is not uncommon for two eggs to mature and be released at about the same time in the same ovulation period. If this happens, each egg is fertilized by a different sperm, which results in fraternal (dizygotic) twins. Fraternal twins are not genetically identical and may or may not be of the same sex. During pregnancy and development they each form their own supporting structures, including a placenta. Jane and John had fraternal twins.
The other type of twins is referred to as identical (monozygotic) twins. They are formed from one egg that is fertilized by one sperm. For identical twins to form, the quickly dividing fertilized cell mass separates into two separate cell masses. Since sex is genetically determined from the combination of the parental chromosomes, identical twins are of the same gender. Monozygotic twins may develop their own separate supporting structures or they may share one set.
In this lesson you will examine the following focusing questions:
- What are the sequences of events and hormonal controls that take place throughout fertilization and embryonic development?
- What major tissues and organs arise from the ectoderm, mesoderm, and endoderm?
- How are twins formed?
 Module 4: Lesson 1 Assignment
Module 4: Lesson 1 Assignment
Your teacher-marked Module 4: Lesson 1 Assignment requires you to submit a response to the following:
- Lab—Comparing Embryonic Structures
- Reflect and Connect Questions
Download a copy of the Module 4: Lesson 1 Assignment to your computer now. You will receive further instructions about how to complete this assignment later in the lesson.
The other questions in this lesson are not marked by the teacher; however, you should still answer these questions. The Self-Check and Try This questions are placed in this lesson to help you review important information and build key concepts that may be applied in future lessons.
After a discussion with your teacher, you must decide what to do with the questions that are not part of your assignment. For example, you may decide to submit to your teacher the responses to Try This questions that are not marked. You should record the answers to all the questions in this lesson and place those answers in your course folder.
You will gain information in this lesson that you can use to complete the Unit B Assessment, the Fertility Case Study. Add information to your course folder as you work through the lesson.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember, you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.4. Page 2
Module 4—From Fertilization to Birth
 Explore
Explore
To begin to understand the changes that occur to the embryo and its supporting structures, including hormonal changes, it is recommended that you first complete the reading below. According to your own learning style, you may choose to make notes, a graphic organizer, a timeline, or another record of your learning. When you have completed the readings, watch the videos to complete your understanding and to learn about some reproductive technologies.
 Read
Read
ectoderm: germ layer that forms hair, nervous system, and skin
mesoderm: germ layer that forms muscle, bone, and muscular organs
endoderm: germ layer that forms gut lining, pancreas, and liver
zygote: the one-celled product of egg and sperm fusion; also known as the fertilized egg
cleavage: cell division in which the zygote divides into smaller, identical cells, called blastomeres, without increasing the total size of the cell mass
blastocyst: embryonic stage that results when the morula hollows out; the outer layer is the trophoblast and becomes the chorion; the inner cell mass becomes the embryonic disc
human chorionic gonadotropin (HCG): hormone released from the chorion after implantation; directs corpus luteum to continue making estrogen/progesterone, thereby maintaining the endometrium and preventing menstruation
gastrulation: the folding and differentiation of the embryonic disc into three germ layers, forming the embryonic stage called the gastrula
primary germ layers: three layers formed during gastrulation—endoderm, mesoderm, and ectoderm
morphogenesis: the development of body organs and structures; begins with gastrulation
differentiation: the turning on and off of genes in a cell; results in specialized cell functions
neurulation: the process of forming the embryo's neural tube, which will develop into the brain and spinal cord
allantois: extra-embryonic membrane that forms the foundation for the umbilical cord, which connects the fetus with the placenta
amnion: extra-embryonic membrane that is a closed, fluid-filled sac surrounding the fetus; protects the fetus from impact and temperature change
chorion: outermost layer of the embryo; develops from the trophoblast layer of the blastocyst; will form the fetal blood pool of the placenta
yolk sac: extra-embryonic membrane that produces first blood cells
placenta: embedded in the endometrium; provides a location where nutrients, gases, and wastes can be exchanged between fetal and maternal blood pools
umbilical cord: tube of blood vessels that connects the fetus to the placenta; for exchange of nutrients, gases, and wastes
ectopic pregnancy: occurs when fertilization and implantation take place in the oviduct
To understand how two gamete cells, each containing half the chromosome number of each parent, can combine and transform into an organism composed of millions of cells within just the first two months of gestation, you need to better understand fertilization, implantation, and embryonic development.
Read pages 508 to 519, “Section 15.1: Fertilization and Embryonic Development”, in the textbook.
Summarize this information according to your preference and learning style. A graph similar to “Figure 15.5” on page 512 of your textbook is helpful in understanding the homeostasis of hormones during pregnancy. A table summarizing the organs and systems that develop from the ectoderm, mesoderm, and endoderm is also useful. Ensure that your work includes descriptions of the following concepts:
- fertilization
- zygote
- cleavage
- blastocyst
- implantation
- human chorionic gonadotropin
- gastrulation
- primary germ layers
- morphogenesis
- differentiation
- neurulation
- allantois
- amnion
- chorion
- yolk sac
- placenta
- umbilical cord
Many complications can arise during prenatal development. One of the first problems that can occur is that implantation in the uterine lining does not successfully take place. Implantation can happen in the oviducts, in other areas of the uterus, or in the abdominal cavity. Such an event is called an ectopic pregnancy.
 Watch and Listen
Watch and Listen
Now that you have been introduced to the concepts and terminology of embryonic development, watch the following videos to gain further understanding of this important prenatal period. As you watch the videos, you may want to add information to your work for your course folder.
1.5. Page 3
Module 4—From Fertilization to Birth
 Lab—Comparing Embryonic Structures
Lab—Comparing Embryonic Structures
Looking at images will help you understand the differences between the stages of embryonic development and the structures that support the embryo. In this lab you will examine microscope slides showing various stages of embryonic development in a sea urchin and you will compare the support structures of an embryonic chick to those of an embryonic human.

© 2008 Jupiterimages Corporation
Early embryonic development is similar in many species. In the beginning, formation of the embryonic cells and the supporting structure cells cannot be distinguished between different species of organisms. Embryos in the early stages of development of a fish, reptile, amphibian, bird, and mammal all seem to be very similar.
In this investigation you will compare embryonic stages of development using a microscope. The images will be provided.
The lab is similar to the one on page 519 of the textbook; however, since you may not have a microscope, various microscope images will be provided for you.
 Module 4: Lesson 1 Assignment
Module 4: Lesson 1 Assignment
Retrieve the copy of the Module 4: Lesson 1 Assignment that you saved to your computer earlier in this lesson. Complete Lab—Comparing Embryonic Structures. Save your completed assignment in your course folder. You will receive instructions about when to submit your assignment to your teacher later in this lesson.
 Self-Check
Self-Check
SC 1. To review the developmental stages of the embryo, complete this drag-and-drop activity about fertilization.
SC 2. Complete this drag-and-drop activity to check your understanding of the events from ovulation to implantation
SC 3. Label the diagram showing the extra-embryonic membranes supporting the developing embryo.
 Self-Check Answers
Self-Check Answers
SC 3.
- chorion
- amniotic cavity
- allantois
- maternal blood vessels
- endometrium
- amnion
- yolk sac
- developing placenta
The extra-embryonic membranes are structures that are external to (extra-) the embryo.
 Discuss
Discuss
In your course discussion area, respond to one, some, or all of the following questions:
D 1. Do you think that there should be special schools for pregnant teens, or should all schools do more to try to accommodate the various needs of these expectant mothers?
D 2. Does an embryo have the use of all its senses in utero?
D 3. How is it possible that different mammalian species develop all of the same organ systems in different time periods? What regulates this process?
D 4. Is it possible for the fetus to learn in utero? If so, what is the possible extent of the learning?
D 5. To what extent can or should humans control and change the characteristics of an embryo?
D 6. How is it possible that the development of litters of four or more offspring happens?
 Self-Check
Self-Check
SC 4. Many important processes, structures, and functions were presented in this lesson. Check your mastery of this information by completing the following questions from your textbook.
- questions 1 to 4, page 509
- questions 5 to 9, page 511
- questions 10 to 14, page 512
- questions 15 to 19, page 515
- questions 20 to 23, page 517
Check the following link to see how well you answered the questions and consult with your teacher about any concerns that you may have.
 Self-Check Answers
Self-Check Answers
SC 4.
- There are 46 chromosomes that make up the zygote (fertilized egg): 23 from the sperm and 23 from the egg.
- The egg must be fertilized within 12 to 24 hours of release because it loses its capacity to develop further after 24 hours.
- The sperm must survive the acidic environment of the female reproductive tract. In addition, only one oviduct contains an egg each month; many of the sperm may enter the "wrong" oviduct.
- It takes the actions of several sperm and their acrosome enzymes to break through the protective jelly-like layer of the egg, so a sperm that arrives after the first few have breached the barrier is able to utilize its own acrosome enzymes to enter successfully.
- Cleavage is cell division without growth. This is the initial stage of mitotic divisions after the formation of the zygote in the oviduct. The cleavage divisions do not increase the size of the zygote. They only increase the number of cells within it.
- The morula reaches the uterus within 3-5 days of fertilization, and upon arrival it begins to fill with fluid that diffuses from the uterus. Within the fluid-filled space inside the morula, two different groups of cells characterize the blastocyst: ones that nourish the embryo and ones that become the embyro.
- It is the inner cell mass that develops into the embryo.
- Implantation occurs when the blastocyst nestles in the endometrium (lining of the uterus). This happens between about the 10th and 14th day after fertilization. The blastocyst attaches to the endometrium by secreting enzymes from the trophoblast cells within to digest some of the tissues and blood vessels.
- hCG is human chorionic gonadotropin hormone, which is secreted to maintain the corpus luteum once implantation has taken place. It is secreted at a high level for the first two months, declining to a low level by the end of four months, when there is a fully functional placenta to take over the production of estrogen and progesterone from the corpus luteum. At this point, the hormone production of the corpus luteum is no longer important, although it continues to exist throughout the pregnancy.
- The amniotic cavity is a space that forms between the inner cell mass and the trophoblast. This space fills with fluid, and this is where the embryo will develop, within the sac known as the amnion.
- The embryonic disk is composed of three layers: the ectoderm, mesoderm, and endoderm.
- The creation of the primary germ layers is called gastrulation. The developing embryo at this point is called the gastrula.
- Morphogenesis, which begins with gastrulation, is a series of events that form the distinct structures of the developing embryo. It depends on the ability of embryonic cells to change into different types of cells.
- The development of the primary germ layers creates three distinct layers of cells: the endoderm, mesoderm, or the ectoderm. The cells in the primary germ layers are the source of all of the organs and tissues of the body. The process of the development of these cells into particular shapes and able to perform particular functions is called differentiation.
- Neurulation is the development of the neural tube (found just above the notochord), which develops into the brain and the spinal cord. Cells along the surface of the notochord begin to thicken. As the cells thicken, folds develop along each side of a groove along this surface. As the folds fuse, they become the neural tube.
- During the third week, a thickened band of mesoderm cells (a primary germ layer) develops along the back of the embryonic disk. These cells lie along what will become the baby's back and come together to form the notochord (the basic framework of the skeleton). In addition, a small reddish bulge that contains the heart forms; the heart begins to beat on the 18th day.
- During the fourth week, the blood cells are forming and beginning to fill the developing blood vessels; the lungs and kidneys are taking shape; small buds which will become limbs form; a distinct head, with early evidence of eyes, ears, and a nose, is visible.
- Students will list any four of the following: In the fifth week, the lidless eyes are open, and the cells of the brain are differentiating very quickly. At the sixth week, the brain is continuing to develop; the limbs are lengthening and can flex; the gonads produce hormones to influence the development of the external genitalia. In the seventh and eighth weeks, the organs are fully formed; the nervous system is coordinating the body activity; a skeleton of cartilage has formed; eyes are well developed, but not open; nostrils are developed but are plugged with mucus; external genitalia are developing, but are undifferentiated at this point. Upon completion of the eighth week, approximately 90 percent of the organs and structures are established, and continue to enlarge and mature.
- The embryo is identified as a fetus ("offspring") after the eighth week of pregnancy, when the organs and structures are established.
- The extra-embryonic membranes are: the allantois, the amnion, the chorion, and the yolk sac.
- One portion of the placenta develops from the chorion. The allantois is the foundation of the umbilical cord.
- The placenta has nutritional, excretory, respiratory, endocrine, and immune functions.
Nutritional: transports nutrients such as glucose, amino acids, and fatty acids; it also stores nutrients (protein, fats, and carbohydrates, minerals) to be released later in the pregnancy.
Excretory: transports wastes such as urea, ammonia, and creatinine from the fetal blood to the mother's blood.
Respiratory: transports oxygen from mother to fetus, and carbon dioxide from fetus to mother.
Endocrine: secretes hormones such as estrogen, progesterone, and human chorionic gonadotropin; allows these hormones to diffuse from mother to fetus and fetus to mother.
Immune: provides passive immunity by transporting antibodies from the mother to the fetus's blood.
- The umbilical cord contains one vein and two arteries; the arteries transport oxygen-depleted blood from the fetus to the placenta. The vein transports oxygen-rich blood to the fetus. (Students can diagram the pathway to summarize the role).
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), TRG Pg 6-42 & 6-43. Reproduced by permission
1.6. Page 3
Module 4—From Fertilization to Birth
 Reflect and Connect
Reflect and Connect
You have read and viewed the many changes that occur throughout embryonic development. Before beginning your lesson assessment, you may choose to practice the review questions on page 518. Your teacher may indicate a selection of questions that would best suit your needs. Discuss your responses with your teacher.
 Module 4: Lesson 1 Assignment
Module 4: Lesson 1 Assignment
Retrieve the copy of the Module 4: Lesson 1 Assignment that you saved to your computer earlier in this lesson. Complete Reflect and Connect. Save your completed assignment in your course folder. You will receive instructions on when to submit your assignment to your teacher later in this lesson.
 Reflect on the Big Picture
Reflect on the Big Picture
No other human growth period shows as much change as that of embryonic development. Understanding what is happening during pregnancy makes most expectant mothers and fathers very aware of the significance of the day-to-day changes and the factors that can affect these changes.
Fertility Case Study Update
So it was with Jane and John. However, when their twins were born, it took a bit more understanding to figure out how their twins could be born with different skin colours. The explanation comes from their parental background. John is of mixed race, and has a Jamaican-English heritage. Jane is of caucasian-Scandinavian background. John’s sperm carry genes for both light and dark skin colour.
José and Maria’s situation was more complicated and had severe results. Maria’s ectopic pregnancy progressed to a point that the Fallopian tube ruptured. The pregnancy was terminated and her seriously damaged tube was removed in surgery. During the surgery, doctors discovered that Maria only had one ovary and one Fallopian tube. The ectopic pregnancy had destroyed Maria’s only oviduct.
 Going Beyond
Going Beyond
The development of the embryo is very complex and consists of much more detail than can be presented in this lesson. Remember that all parts of the embryo, and later the fetus, develop from one cell. As cells divide and the organism grows, the cells differentiate and congregate to form all of the specialized structures of the body. If you are interested in this field of study, research how specific structures, such as the eyes, ears, muscles, or bones, are formed.
There are many other terms that define specific processes occurring during embryonic development. You may choose to research the meaning of the following terms:
- organogenesis
- neurogenesis
- angiogenesis
- chondrogenesis
- myogenesis
- osteogenesis
- zygocity
- fourth germ layer
You may also wish to research the Carnegie stages of development, in which each stage is defined through the embryo’s external and internal development. Your research could include how embryonic cells communicate to each other.
 Module 4: Lesson 1 Assignment
Module 4: Lesson 1 Assignment
Submit your completed Module 4: Lesson 1 Assignment to your teacher for assessment.
1.7. Page 4
Module 4—From Fertilization to Birth
 Lesson Summary
Lesson Summary
This lesson addressed the following focusing questions:
- What are the sequences of events and hormone controls that occur throughout fertilization and embryonic development?
- What major tissues and organs arise from the ectoderm, mesoderm, and endoderm?
- How are twins formed?
Prenatal development is divided into two main periods. The first period takes place from fertilization to the end of the eighth week of development. This period is called embryonic development, and the developing offspring is referred to as the embryo during this time. The period that takes place from the beginning of the ninth week to birth is called the fetal development period, and the offspring is referred to as the fetus during this time.
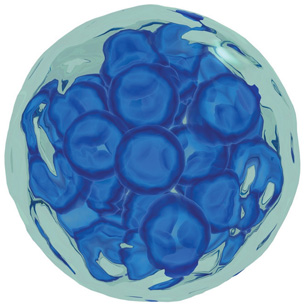
Once the egg and sperm have been correctly formed and released, both must meet inside the female’s reproductive system for natural fertilization to occur. The process of the sperm entering the egg thus combining the 23 chromosomes from the father’s sperm and the 23 chromosomes from the mother’s egg, is known as fertilization. Fertilization occurs in the oviduct, or Fallopian tube. Fertilization results in a single cell with 46 chromosomes, now called a zygote. While still in the oviduct, the zygote begins to divide through the process of cleavage, and at the 16 cell stage it is classified as a morula. The morula continues to divide and begins to fill with fluid. The resulting structure is then called a blastocyst.
The blastocyst forms two distinct layers of cells, an outer layer called the trophoblast, which will develop into the supportive membrane structure called the chorion. The mass of inner cells of the blastocyst will form the embryo. As the blastocyst reaches the uterus, the trophoblast produces and secretes an enzyme that digests some of the endometrial tissue, enabling the blastocyst to implant itself in the uterine lining.
As implantation is being completed, the amniotic cavity develops within the amnion,a type of sac. From the amniotic cavity, the embryonic disc forms. This disc will undergo the process of gastrulation—the formation of germ tissue layers (endoderm, mesoderm, and ectoderm). The event of gastrulation gives rise to a new term for the developing offspring, a gastrula. During gastrulation a series of changes occurs where cells begin differentiating.
Tremendous growth and organ development happen in the first trimester, with 90% of all organs being formed by the end of the embryonic period. At the same time as the embryonic growth is happening, supporting structures are also developing. The allantois, amnion, chorion, and yolk sac are formed to support the developing embryo and, later, the fetus. Some of these structures then give rise to the placenta and umbilical cord. The supporting structures help to nourish, protect, and remove wastes from the developing offspring during prenatal development. Once the baby is born, all of the supporting structures are expelled from the female’s body. These structures are then collectively referred to as the afterbirth.
Lesson Glossary
allantois: extra-embryonic membrane that forms the foundation for the umbilical cord, which connects the fetus with the placenta
amnion: extra-embryonic membrane that is a closed, fluid-filled sac surrounding the fetus; protects the fetus from impact and temperature change
blastocyst: embryonic stage that results when the morula hollows out; the outer layer is the trophoblast and becomes the chorion; the inner cell mass becomes the embryonic disc
chorion: outermost layer of the embryo; develops from the trophoblast layer of the blastocyst; will form the fetal blood pool of the placenta
cleavage: cell division in which the zygote divides into smaller, identical cells, called blastomeres, without increasing the total size of the cell mass
differentiation: the turning on and off of genes in a cell; results in specialized cell functions
dizygotic twins: twins that form when two eggs are fertilized by two sperms; also known as fraternal twins; may be of different sexes
ectoderm: germ layer that forms hair, nervous system, and skin
ectopic pregnancy: occurs when fertilization and implantation take place in the oviduct
embryo: the organism in the stages of development from the time the zygote begins cleavage until nine weeks of gestation, when the embryo becomes a fetus
endoderm: germ layer that forms gut lining, pancreas, and liver
extra-embryonic membranes: membranes surrounding the embryo, and later the fetus, that support its development in different ways; include the allantois, amnion, chorion, and yolk sac
fertilization: the fusing of a sperm nucleus with an egg nucleus to form a zygote; occurs in the oviduct
fetus: the organism in the stages of development from nine weeks until birth
gastrulation: the folding and differentiation of the embryonic disc into three germ layers, forming the embryonic stage called the gastrula
human chorionic gonadotropin (HCG): hormone released from the chorion after implantation; directs corpus luteum to continue making estrogen/progesterone, thereby maintaining the endometrium and preventing menstruation
implantation: burrowing of the blastocyst into the wall of the endometrium of the uterus
mesoderm: germ layer that forms muscle, bone, and muscular organs
monozygotic twins: identical twins formed when the embryonic mass produced by the union of one egg and one sperm splits into two separate, identical masses; are of the same sex
morphogenesis: the development of body organs and structures; begins with gastrulation
morula: embryonic stage of a solid ball of identical cells that results from cleavage of the zygote
neurulation: the process of forming the embryo's neural tube, which will develop into the brain and spinal cord
placenta: embedded in the endometrium; provides a location where nutrients, gases, and wastes can be exchanged between fetal and maternal blood pools
primary germ layers: three layers formed during gastrulation—endoderm, mesoderm, and ectoderm
umbilical cord: tube of blood vessels that connects the fetus to the placenta; for exchange of nutrients, gases, and wastes
yolk sac: extra-embryonic membrane that produces first blood cells
zygote: the one-celled product of egg and sperm fusion; also known as the fertilized egg
1.8. Lesson 2
Module 4—From Fertilization to Birth
Lesson 2—Fetal Development, Trimester Events, and Environmental Factors
 Get Focused
Get Focused

©TheBand / Shutterstock
The process of prenatal development continues after the embryonic period. In Lesson 1, you learned how in embryonic development, an offspring progresses from a single cell to an organism of millions of cells in a period of just two months. At the beginning of the ninth week of prenatal development, the name embryo is dropped, and the developing offspring is now called a fetus. As the embryo went through morphogenesis, the bases of all of the organ systems were formed. During the fetal stage, the organ systems develop further or mature. The placenta and umbilical cord are almost completely formed by the ninth week, and will soon take over hormonal control of maintaining the pregnancy.
Even though prenatal development is divided into the embryonic and fetal development periods, the full pregnancy is divided into three trimesters—each
trimester is three-months in duration. The first trimester consists of the embryonic development period and the beginning of fetal development. The first three months are the most critical because the bases of all of the organ systems are formed during this time. The heart begins beating; blood cells flow through blood vessels; limbs are formed; genitals are now present; and the brain, sense organs, and nervous tissue are formed.
© shahar choen/Shutterstock
trimester: one-third of the gestational period
There are three trimesters of pregnancy.
The second and third trimesters also have significant developmental events consisting of further system development and maturation. A timeline of some major developments follows.
End of Month 4
- The baby is developing reflexes, such as sucking and swallowing, and may begin sucking his or her thumb in utero.
- Tooth buds are developing.
- Sweat glands are forming on the baby’s palms and soles.
End of Month 5
- Hair begins to grow on the baby’s head.
- Eyebrows, eyelids, and eyelashes appear.
End of Month 6
- The baby’s skin is covered with a protective coating called vernix.
- The baby is able to hiccup.
vernix: a cheesy, oily substance covering the fetus; has antibacterial properties

© Noel Powell/123RF Limited
End of Month 7
- Taste buds have developed.
- Fat layers are forming.
End of Month 8
- Tremendous brain growth occurs at this time.
- The baby’s fingernails may now extend beyond the fingertips.
- Most body organs are now developed, except for the lungs.
End of Month 9
- The lungs are mature.
- The baby is now fully developed and can survive outside the mother’s body.
teratogen: a substance that can cause deformities during fetal development; can be chemicals, viruses, or radiation
Substances and circumstances can affect prenatal development at any time. However, it is during the first trimester when the developing offspring is most vulnerable to teratogens, which are substances or other factors that can alter normal development. Some examples of teratogens are cigarette smoke, alcohol, drugs, and x-rays. There are a host of others.

© Lee O’Dell/shutterstock
In addition to harmful agents that may be transferred to the embryo and fetus, there are also substances that are essential for proper growth and development. Proper nutrition, which includes the right amounts of vitamins and minerals, is fundamental to the healthy development of the embryo and fetus. For example, sufficient amounts of Vitamin B9, also known as folate or folic acid, help prevent neural tube defects during embryonic and fetal development. One of the activities you will be asked to do in this lesson will help you understand why it is important for a woman to consume a high amount of folate in her diet before conception.

© Tyler Hartl/shutterstock
folic acid (folate): Vitamin B9; ingestion prior to and during pregnancy prevents neural tube defects, such as spina bifida

© Gelpi/shutterstock
Case Study Update:
Although Jane and John did not have to undergo hormone therapy or other reproductive enhancement technologies discussed in Module 3, you did advise them on the significance of knowing when ovulation was taking place. Ovulation is the time when the egg is most receptive to fertilization. Jane’s urine and blood tests now indicate a high level of hCG. This high hormone level is the basis of the pregnancy test and is what confirms a pregnancy. Fertilization has thus been successful and the embryo has begun development.
In Lesson 2 you will examine the following focusing questions:
- What are the major events of each trimester?
- What is the significance of the first trimester?
- What is the significance of the effects of teratogens on embryonic and fetal development?
This lesson will take approximately 40 minutes.
 Module 4: Lesson 2 Assignment
Module 4: Lesson 2 Assignment
Your teacher-marked Module 4: Lesson 2 Assignment requires you to submit a response to questions regarding genetic, hormonal, and environmental factors and their effects on embryonic and fetal development.
Download a copy of the Module 4: Lesson 2 Assignment to your computer now. You will receive further instructions on how to complete this assignment later in the lesson.
You must decide what to do with the questions that are not marked by the teacher.
Remember, that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.9. Page 2
Module 4—From Fertilization to Birth
 Explore
Explore
fetal alcohol spectrum disorder: a permanent syndrome of birth defects caused by maternal intake of alcohol during pregnancy; includes disorders of growth, behaviour, and cognitive abilities
lactation: the production and secretion of milk from the breast; also known as “nursing”
parturition: childbirth or labour
To understand fetal development, complete the Read and Watch and Listen activities. You may choose the order in which you complete the activities. As you work through the material, record the information in your course folder. Include the concepts of teratogens, fetal alcohol spectrum disorder, parturition, and lactation in your work. Consider the significance of “Figure 15.12” on page 522 of the textbook.
 Read
Read
Understanding the events of embryonic and fetal development and how substances and other factors can help or be harmful to prenatal development will be better understood after you read from the start of page 520 up to the heading “Parturition: Delivery of the Baby” on page 523 in your textbook. Also, take the time to do an Internet search using the search words “fetal development” for more information.
 Watch and Listen
Watch and Listen
Watch the following videos to gain a better understanding of the events of fetal development.
- The “Fetal Development and Birth: An Amazing Transformation” video outlines the development of fetal systems during each trimester and identifies the hormones and genetic factors involved in regulating fetal development. It also illustrates the mechanism for exchanging nutrients and wastes between the mother and fetus, and describes environmental influences, such as alcohol and drugs.
You may be required to enter a username and password to access the video. Contact your teacher for this information.
For an illustrated presentation of the pregnancy timeline, do a web search using the search terms “pregnancy timeline” “and “aboutkidshealth.” Click on “Pregnancy and Babies: Fetal Development.”
- This video reviews the pregnancy timeline from fertilization and implantation through to full-term fetal development.
 Try This
Try This
TR 1. Ensuring proper nutrition is just as important as staying away from harmful teratogens when pregnant. Read “Thought Lab 15.1: Folic Acid and Neural Tube Defects” on page 524 of your textbook. Answer the “Analysis” questions and then check your answers with your teacher to see how well you understand the importance of the need for folic acid.
TR 2. See how well you know the major events of prenatal development by completing this drag-and-drop activity.
 Discuss
Discuss
Discuss one, some, or all of the following questions in the discussion area for your class.
D 1. Why are most women who wish to become pregnant told by their doctor to take a prenatal vitamin supplement?
D 2. There are many teenage pregnancies every year in Canada. Do you see a possible problem with some teenage dietary habits and teenage pregnancy?
D 3. Can you think of any everyday household substances that pregnant mothers should stay away from?
D 4. Why should pregnant women not change cat litter boxes?
 Self-Check
Self-Check
SC 1. See how well you understand fetal development by answering questions 24 to 26 on page 520 and questions 27 and 28 on page 523 of your textbook. Discuss your answers with your teacher.
 Self-Check Answers
Self-Check Answers
Textbook questions 24 to 26, page 520
- The main difference between the embryonic and fetal development periods relate to the type of development of the organism. The embryonic period is a time of morphogenesis when the organs are formed. During the fetal period the organs continue to develop.
- You can list any three of the following events during the second trimester:
- heartbeat can be heard with a stethoscope
- the bones of the skeleton and joints begin to form
- face begins to look distinctly human
- the brain grows rapidly
- the nervous system begins to function
- the mother can feel fetal movements as the limbs grow and develop
- fetus becomes covered with fine soft hair and an oily substance
- skin becomes more pink as capillaries extend into it
- body becomes larger in relation to the head
- the scalp develops hair
- eyes open
- eyelashes form
- fetus assumes “fetal position”
- heartbeat can be heard with a stethoscope
- Students can list any three of the following events during the third trimester:
- brain cells form rapidly
- testes descend in males
- fat develops beneath the skin
- fetus shifts to head-first position
- bone marrow takes over production of red blood cells
- the digestive and respiratory systems mature
- lanugo is shed
- brain cells form rapidly
Textbook questions 27 and 28, page 523
- Teratogens are agents that cause structural abnormalities due to exposure during pregnancy.
- Examples of dangers that teratogens pose include:
- structural abnormalities, such as deformed limbs (prescription medication, e.g., Thalidomide)
- constriction of blood vessels, restricting oxygen supply and increasing risk of underweight babies, premature birth, stillbirth, and miscarriage (cigarette smoke)
- damage to the brain, central nervous system, and physical development, leading to decreased weight, height, head size, capacity to learn, memory problems, and personality disorders (alcohol)
- excess amounts of vitamin C consumed by the mother can result in the baby being prone to scurvy, easy bruising, and infections
- increased danger of miscarriage, low birth-weight babies, difficulty fighting infection and disease, developmental delay (exposure to environmental contaminants)
- structural abnormalities, such as deformed limbs (prescription medication, e.g., Thalidomide)
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), TRG Pg 6-47. Reproduced by permission
1.10. Page 3
Module 4—From Fertilization to Birth
 Reflect and Connect
Reflect and Connect
Prenatal development extends through the embryonic period and the fetal stage, Reflect on the significance of the three trimesters and the events of each trimester. Consider the influence of teratogens during the first trimester and how they can have permanent effects on the developing child.
Record in your course folder any information from this lesson that could be relevant to your work on the Fertility Case Study.
 Module 4: Lesson 2 Assignment
Module 4: Lesson 2 Assignment
Retrieve the copy of the Module 4: Lesson 2 Assignment that you saved to your computer earlier in this lesson. Complete the assignment.
You will receive instructions on when to submit your assignment to your teacher later in this lesson.
 Reflect on the Big Picture
Reflect on the Big Picture
When a couple wanting children discovers that they are pregnant, it is an awesome and exciting journey to birth. However, many expecting couples choose to wait until the pregnancy is at least three months along, or until the end of the first trimester, before they announce the pregnancy to friends and family. This time frame corresponds to the completion of embryonic development and the first month of fetal development. This is the most crucial period of the pregnancy. Most miscarriages happening within the first 13 weeks of a pregnancy are due to chromosomal abnormalities that prevent normal embryonic and fetal development. Waiting until after the thirteenth week to announce a pregnancy often saves the discomfort of having to answer questions about the pregnancy if the baby is lost. However, miscarriages still occur beyond thirteen weeks, and a stillbirth can occur at full term. There are many hazards on the journey to birth.
Fertility Case Study Update
Jane and John had their pregnancy confirmed and were able to get through the first 13 weeks with no complications. Because Jane and John knew that they wanted to conceive, Jane had been watching her nutritional requirements and her exposure to any harmful substances.
 Going Beyond
Going Beyond
There are so many complications that can affect prenatal development. One of the most common developmental problems is premature birth, in which fetal development is not completed to full term. Do research on premature birth to answer some, or all, of the following questions.
- How small can a baby be and still survive outside the womb?
- What are some of the complications for babies that are born early?
- How are preemies cared for immediately following birth, and then a few weeks after birth?
- What is “kangaroo care” for preemies?
- Are there any residual complications of premature birth that can carry over into later childhood or adulthood?
 Module 4: Lesson 2 Assignment
Module 4: Lesson 2 Assignment
Submit your completed Module 4: Lesson 2 Assignment to your teacher for assessment.
1.11. Page 4
Module 4—From Fertilization to Birth
 Lesson Summary
Lesson Summary
The following focusing questions were addressed in this lesson:
- What are the major events of each trimester?
- What is the significance of the first trimester?
- What is the significance of the effects of teratogens on embryonic and fetal development?
Prenatal development is divided into three trimesters and two developmental periods. Embryonic development begins at fertilization and ends after about the eighth week of pregnancy. Fetal development begins at the ninth week and continues until birth. Both embryonic and the first events of fetal development occur within the first trimester. The first trimester is the time when the developing embryo and, later, the fetus are most vulnerable to improper nutritional requirements and exposure to harmful teratogenic agents. This is the time when the most sensitive embryonic and fetal development is taking place. The fetal development period consists of significant events related to the progressing months of pregnancy. Most of the fetal development period is occupied by further development of the organ systems. Understanding the significant developmental events that occur during pregnancy helps doctors and parents follow the development of the maturing fetus right up until birth.
Refer to “Table 15.2” on page 521 of the textbook for a review of the major events in prenatal development.
Lesson Glossary
fetal alcohol spectrum disorder: a permanent syndrome of birth defects caused by maternal intake of alcohol during pregnancy; includes disorders of growth, behaviour, and cognitive abilities
folic acid (folate): Vitamin B9; ingestion prior to and during pregnancy prevents neural tube defects, such as spina bifida
lactation: the production and secretion of milk from the breast; also known as “nursing”
parturition: childbirth or labour
prenatal: before birth
teratogen: a substance or other factor that can cause developmental abnormalities during fetal development; e.g., chemicals, viruses, or radiation
trimester: one-third of the gestational period
There are three trimesters of pregnancy.
vernix: a cheesy, oily substance covering the fetus; has antibacterial properties
1.12. Lesson 3
Module 4—From Fertilization to Birth
Lesson 3—Hormones and the Birthing Process
© Jonathan Cooke/Shutterstock
 Get Focused
Get Focused
Birth is an incredible event. Although birth is not the beginning of your life’s story, it is certainly one of the most important moments in your life. What is your birth story? Do you know what happened around the time of your birth? What was the day of your birth like? What events surrounded this special moment in your life?

© Phase4Photography/Shutterstock
Today women have many choices for how to deliver their baby. Birth at home with a midwife, birth at a birthing centre with a midwife, birth in a hospital, water birth, and many more options are available today. No matter what a woman’s birth plan is, once the birthing process begins there is no going back.
Gestation in the human species is approximately 266 days and ends with the birth of the fetus. For Jane, a few days before her baby was ready to enter the outside world, she felt a sensation that the baby was settling deeper into her pelvis. This sensation is commonly called lightening.
Parturition, or labour, is divided into three stages: the dilation stage, the expulsion stage, and the placental stage. Jane was said to be in labour when her cervix was dilated to about 3 cm in diameter and her uterine contractions lasted for 40 seconds and occurred every 15 to 20 minutes.
dilation stage: the stretching and opening of the cervix to 10 cm to allow passage of the fetus during expulsion
expulsion stage: the stage in which the smooth muscle walls of the uterus contract in rhythmic cycles to deliver the fetus from the vagina
placental stage: the stage in which further uterine contractions push the placenta out of the body through the vagina; also known as delivery of the afterbirth
dilation: the opening of the cervix to allow passage of the baby
contractions: the rythmic shortening of the muscles of the uterus to expel the baby

© emin kuliyev/Shutterstock

© Ingvald Kaldhussater/Shutterstock

© Vivid Pixels/Shutterstock
Jane’s labour was controlled by both nerves and hormones through a positive feedback system. The dilation stage of parturition began as the cervix shortened, contracting up into the uterus. This event stimulated the secretion of oxytocin from the pituitary’s posterior lobe. Oxytocin caused uterine contractions, which pushed the fetus down toward the cervix. The pressure of the fetus on the cervix caused the cervix to stretch. These events sustained positive feedback to the posterior pituitary, causing the continued release of oxytocin. Uterine contractions also stimulated the release of prostaglandins, another example of positive feedback.
prostaglandins: a group of hormones that contribute to parturition by thinning the cervix and increasing contraction of the uterus
The expulsion stage of parturition consists of the delivery of the fetus. This is the stage in which Jane and John’s baby was actually born. For this to happen, their baby’s head had to rotate as it moved into the birth canal. Once the head and shoulders of the baby were out of the birth canal, the rest of the body delivered quickly. Soon after delivery, John was able to cut the umbilical cord.

© Francois Etienne du Plessis/Shutterstock
There are many reasons why a normal vaginal birth may not be possible. When this happens, doctors deliver the baby by Cesarean section. A C-section, as it is sometimes called, is a surgical procedure where an incision is made in the mother’s lower abdomen through to her uterus.
Caesarean section (C-section): a surgical procedure in which the fetus is removed from the abdomen through an incision; used when vaginal birth is difficult or impossible

© PhotoCreate/Shutterstock
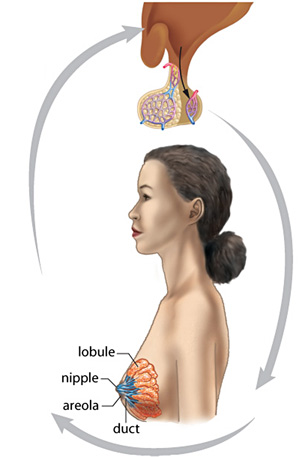
Lactation, or breast-feeding, occurs when estrogen and progesterone production is suppressed and the anterior pituitary secretes the hormone prolactin. Breast milk production is stimulated by the suckling of the new baby, through nerve endings in the nipple. Nervous stimulation causes oxytocin to be secreted, which acts to cause contractions in the breasts. For the first few days of breast-feeding, Jane produced colostrums, a yellowish liquid that contains antibodies and more protein than breast milk.

© PhotoCreate/Shutterstock
sucking reflex: an instinctive sucking action by a newborn that stimulates oxytocin secretion in the mother; results in release of milk from the mammary glands into the milk ducts of the breast
In the placental stage, which in most cases happens within 30 min of the baby’s delivery, the placenta disengages from the uterus and is expelled from the body. Jane was encouraged to breastfeed her baby as soon after delivery as possible. The sucking reflex also establishes positive feedback, causing the muscular uterine wall to contract. The shrinking of the uterus reduces blood loss.

© Trutta55/Shutterstock
The following focusing questions are addressed in this lesson:
- What triggers the birthing process and what are its stages?
- What controls lactation?
 Module 4: Lesson 3 Assignment
Module 4: Lesson 3 Assignment
There is no assignment for this lesson. The information from this lesson will be assessed in your module assessment.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember, you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses is excellent preparation for the Diploma Exam.
1.13. Page 2
Module 4—From Fertilization to Birth
 Explore
Explore
To understand the events of labour, parturition, and lactation, complete the following Read and Watch and Listen activities. According to your personal learning style, you may choose to prepare notes, flow charts, or diagrams to summarize this information. Make sure you save the answers to the following Self–Check activities in your course folder. These feedback loops are an excellent way to summarize information.
 Read
Read
Read “Parturition: Delivery of the Baby” on pages 523 to 526 of the textbook.
 Watch and Listen
Watch and Listen
To review the concepts of this Module, watch the video, “Fetal Development and Birth: An Amazing Transition.” Pay particular attention to the roles of nerve stimulation and hormone control in both parturition and lactation. Use the information from the video to complete your notes. You may be required to enter a username and password in order to view the video. Contact your teacher for this information.
 Self-Check
Self-Check
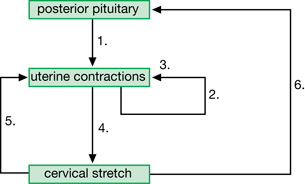
SC 1. Label the following positive feedback mechanism of hormonal control of parturition. File your work in your course folder.
Positive Feedback Mechanisms Controlling Parturition
SC 2. Label the following feedback loop of the mechanism for milk production and lactation.
Milk Production and Secretion
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 526, fig. 15.16. Reproduced by permission.
 Self-Check Answers
Self-Check Answers
SC 1.

This diagram outlines positive feedback mechanisms that are believed to control parturition. Despite advances in technology, understanding of the factors that initiate and control parturition in humans remains incomplete.
SC 2.
Milk Production and Secretion Answer Key

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 526, fig. 15.16. Reproduced by permission.
 Discuss
Discuss
In your course discussion area, discuss one, some, or all of the following questions.
D 1. Why do many women choose to give birth in water?
D 2. How do you feel about men becoming impregnated? (Yes, it is happening.)
D 3. How would a man deliver a baby?
D 4. What is a wet nurse, and why were they used?
D 5. Present technology allows for conception and birth to be controlled. What are the advantages and disadvantages of controlling these processes?
 Self Check
Self Check
Did you know that the greatest number of children born to one woman is 69? In the 1700s a woman from Russia had 16 sets of twins, 7 sets of triplets, and 4 sets of quadruplets!
SC 3. Check your understanding of parturition and lactation by completing questions 29 to 32 on page 526 of your textbook.
 Self-Check Answers
Self-Check Answers
29. During parturition (birth), estrogen and progesterone levels drop and prostaglandins cause the release of oxytocin (these two hormones result in uterine contractions).
30. A Caesarian section is a surgical procedure where the mother's abdomen and uterus are opened so that the baby can be delivered when a natural birth is unsafe. (A Caesarian section may be required if the mother has an STI, or if the mother has a small pelvis, or if the baby is in breech position or has the umbilical cord wrapped more than once around its neck.)
31. Lactation is the formation and secretion of breast milk in the mother.
32. Oxytocin causes contractions in the mammary lobules, enabling the mother's milk to flow to the milk ducts.
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), TRM Pg 526. Reproduced by permission.
1.14. Page 3
Module 4—From Fertilization to Birth
 Reflect and Connect
Reflect and Connect

© Peter Hansen/shutterstock
Did you find out your birth story? Hopefully, you were able to gain an understanding of the events surrounding your birth. Actress Jamie Lee Curtis had a ritual of having her mother tell her the story of her birth every year on her birthday. Young children love hearing over and over about how they were born. The events of your birth story, or anyone else’s, are memories that many people want to keep—some even record the process in home videos.
To ensure your understanding of embryonic and fetal development up to and including birth, you may choose to complete the questions on page 528 of your textbook. Your teacher may indicate which questions are suited to your needs. Discuss your responses with your teacher.
 Reflect on the Big Picture
Reflect on the Big Picture
Fertility Case Study Update
Jane and John have been successful in having a baby. Unfortunately, Karl and Olga and Maria and José have not been able to have a successful pregnancy to date. Each of these couples will have to make choices about how to have a family. Normal conception is not an option for them, but there are many technologies available to assist with conception and the maintenance of a successful pregnancy.
 Going Beyond
Going Beyond
With every birth there is a possibility of conditions arising that are not typical. There is always a chance that the birthing process will not go exactly according to plan. You may wish to research one of the following options:
Option 1
Research the following terms or phrases relating to childbirth:
- effacement
- mucous plug
- Braxton-Hicks contractions
- latent phase
- malpresentation of the fetal head
- being born in the caul
- epidural
- breech birth
- episiotomy
- Apgar score
Option 2
Research how various Aboriginal cultures dealt with childbirth.
 Module 4: Lesson 3 Assignment
Module 4: Lesson 3 Assignment
There is no assignment for this lesson.
1.15. Page 4
Module 4—From Fertilization to Birth
 Lesson Summary
Lesson Summary

© Jiri Vaclavek/Shutterstock
The following focusing questions were addressed in this lesson:
- What triggers the birthing process and what are its stages?
- What controls lactation?
Parturition is divided into three stages, although the events occur as a continuous process. Labour is separated into the dilation stage (uterine contractions begin), the expulsion stage (delivery of the fetus), and the placental stage (the discharge of the placenta).
Labour is initiated and sustained through nervous and hormonal control. Oxytocin and prostaglandin stimulation works through a positive feedback mechanism to promote further uterine contractions. Uterine contractions force the fetus down to the cervix and out through the birth canal. They also cause the placenta to be expelled from the body after birth. If a normal vaginal birth is not possible, it is common for delivery of the fetus to occur through a Cesarean section.
Once the fetus is delivered, it can no longer rely on its mother for air, food, or the elimination of its wastes. All of the baby’s body systems that perform these functions now begin working independently. For the infant to acquire nutrition, it needs to be breast or bottle fed. In breast feeding, the hormone prolactin causes the production of breast milk. The release of oxytocin due to suckling stimulation causes the mammary glands to secrete breast milk.
The desired end result of this reproductive process filled with development and change is the glowing face of a healthy newborn baby.
Lesson Glossary
Caesarean section (C-section): a surgical procedure in which the fetus is removed from the abdomen through an incision; used when vaginal birth is difficult or impossible
colostrum: a rich, yellow secretion from the mammary glands that occurs for two to three days prior to the first secretion of milk; contains mother’s antibodies to protect the newborn from disease
contractions: the rythmic shortening of the muscles of the uterus to expel the fetus
dilation: the opening of the cervix to allow passage of the baby
dilation stage: the stretching and opening of the cervix to 10 cm to allow passage of the fetus during expulsion
expulsion stage: the stage in which the smooth muscle walls of the uterus contract in rhythmic cycles to deliver the fetus from the vagina
parturition: the process of labour and delivery, which is divided into dilation, expulsion, and placental stages
placental stage: the stage in which further uterine contractions push the placenta out of body through the vagina; also known as delivery of the afterbirth
prostaglandins: a group of hormones that contribute to parturition by thinning the cervix and increasing contraction of the uterus
sucking reflex: an instinctive sucking action by a newborn that stimulates oxytocin secretion in the mother; results in release of milk from the mammary glands into the milk ducts of the breast
1.16. Lesson 4
Module 4—From Fertilization to Birth
Lesson 4—Reproductive Technologies: Enhancing or Reducing Fertility, Monitoring Development, and Use in Parturition
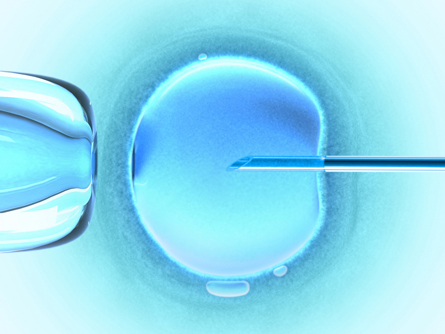
© iDesign/shutterstock
 Get Focused
Get Focused
Humans have been trying to control their reproductive potential for thousands of years. Some of the earliest known reproductive technologies were contraceptive practices dating back to 1550 BC. “According to an ancient medical manuscript called the Ebers Papyrus (1550 BC), women were advised to grind together dates, acacia (a tree bark), and a touch of honey into a moist paste, dip seed wool into the sweet gel and place it in the vulva. As primitive as this sugary mix appears, it was usually effective. Acacia eventually ferments into lactic acid, a well known spermicide.” This quote, along with a host of additional contraceptive information and displays, are at The History of Contraception Museum in Toronto, Canada. This world renowned, one-of-a-kind museum has over 600 different forms of contraceptives.
reproductive technology: any application of human intelligence that increases or decreases reproductive potential

© ZTS/shutterstock
Reproductive technology now includes much more than just contraceptives. In this lesson reproductive technologies are divided into three broad groups: enhancing or reducing fertility, monitoring development, and use in parturition. Many more technologies than can be studied in this lesson are available.
The following focusing question is addressed in this lesson:
- What technologies are used to assist fertilization, to monitor development, and to facilitate parturition?

© Tomasz Trojanowski/shutterstock
 Module 4: Lesson 4 Assignment
Module 4: Lesson 4 Assignment
There is no assignment for this lesson. The information from this lesson will be assessed in the Module Assessment.
Because this is the last lesson of Module 4, at the end you will need to submit the Module Assessment, which is the preparation based on your answers to the five Module Assessment questions presented in the Big Picture. When you have completed Lesson 4, go to the Module Summary and Assessment page for information on the assignment and a marking rubric.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember, you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.17. Page 2
Module 4—From Fertilization to Birth
 Explore
Explore
It seems that humans are quite concerned with ensuring the right timing of fertility. The possibility of having a child when not ready has driven research into how to temporarily reduce reproductive potential. Some of the oldest research is in controlling reproductive potential.
abstinence: not having sexual intercourse; is often practised in order to prevent pregnancies and decrease the risk of transmitting or receiving STIs
barriers: any chemical or physical device that stops sperm from meeting the egg
Examples of barriers include spermicides and condoms.
contraceptive hormone treatment: birth control pills, birth control patches, and injections using estrogen-progesterone combinations to suppress ovulation, thus preventing pregnancy
Examples of technologies that reduce reproductive potential are abstinence, tubal ligation, vasectomy, physical and chemical barriers, and natural family planning. Contraceptive hormone treatment, another technology that reduces the possibility of conception, was used by Maria when she began taking birth control pills, and then again when both she and José were placed on the hormone Clomid.
family planning: natural birth control that consists of avoiding sex during the fertile period around ovulation; can be tested for by a small increase in core temperature; not very effective
tubal ligation: permanent female sterilization in which the Fallopian tubes (oviducts) are cut and sealed to prevent further ova from passing from the ovaries to the site of fertilization
vasectomy: permanent male sterilization in which the ductus deferens are cut and sealed to prevent sperm from passing from the epididymis into the semen

© Monkey Business Images/shutterstock
Technologies that enhance reproductive potential are some of the most advanced of all the assisted reproductive technologies. Because infertility, or sterility, can happen for a wide range of reasons, and the desire for many couples and individuals to have children is so strong, much research has gone into the development of fertility-enhancing technologies. Technologies such as artificial insemination, in vitro fertilization, surrogate motherhood, ovulation test kits, and super-ovulation all assist in bringing forth new offspring.
artificial insemination: a procedure in which semen from a donor is inserted by syringe into the vagina of a receptive female; used in the case of male infertility
in vitro fertilization (IVF): a process in which multiple eggs harvested from a female are combined with sperm in the lab, and the resulting embryo is implanted into the female; used in cases of female infertility
ovulation test kits: home kits that test the urine for a surge in LH, which indicates that ovulation will occur shortly; used to time intercourse to maximize the chances of conceiving
superovulation: hormones similar to FSH are prescribed to stimulate the ovary to produce eggs more consistently
surrogate motherhood: the process by which an embryo is inserted into the uterus of a woman who will carry the fetus to term, then return the baby to the biological parents; used when a woman cannot undergo pregnancy
home pregnancy test: a urine test that indicates if HCG is present in the urine
Before conception even takes place, technologies, such as at-home fertility test kits, are available to help a couple determine their reproductive potential and determine the optimal time to try conceiving. Another technology is a home pregnancy test, which can be purchased from a drug store. A home pregnancy test measures levels of pregnancy hormone in a woman’s urine. In addition to doing a home pregnancy test, more definitive urine and blood tests should be done at a medical laboratory in order to confirm conception.

© Zsolt Nyulaszi/shutterstock
Once it is confirmed that conception has occurred, other technologies are needed to monitor the events of embryonic and fetal development. Ultrasonography is a common technology used to monitor a pregnancy. Fetal surgery is a last-resort technology used to treat certain life-threatening congenital abnormalities. Other technologies that can be used to understand genetic conditions of the fetus are cordiocentesis, amniocentesis, and chorionic villi sampling. The last two technologies will be discussed in Unit C.
amniocentesis: a fetal diagnostic technique done by inserting a syringe through the mother’s abdominal and uterine walls to extract a sample of amniotic fluid, which contains sloughed-off embryonic cells; used to karyotype the embryo and diagnose chromosome non-disjunctions, such as Down’s syndrome
chorionic villi sampling (CVS): a fetal diagnostic technique done by pinching off a small sample of chorionic villus; sample is obtained vaginally
Because chorion cells are embryonic, cells can be karyotyped to diagnose chromosomal non-disjunctions, such as Down’s syndrome.
cordiocentesis: the process of sampling fetal blood from the umbilical cord to test for the possibility of infection or blood disease
Ultrasonography: fetal diagnostic technique by which high-frequency sound waves are bounced off the fetus, providing images of internal and external fetal structures; commonly called ultrasound
Reproductive technologies can also be used in parturition. One such technology has already been discussed—delivery by Caesarian-section. Various technologies are used to assist with the birthing process itself. These include the following:
- induction medication (oxytocin drip)
- fetal heart monitor
- epidural
- episiotomy
- forceps
- suction
A reproductive technology needed shortly after childbirth is related to the Rh factor studied in Biology 20. If the mother is Rh– and the fetus being born is Rh+ , then an anti-Rh antibody is given to the mother within the first 72 hours following childbirth. The injected anti-Rh antibodies destroy any of the baby’s red blood cells that may be in the mother’s blood before the mother’s immune system produces antibodies. Timing of the injection is crucial because it must be done before the mother has started to produce antibodies.
You may choose to review these concepts by turning to page 297 of your textbook and examining "Figure 8.31."
© Ewa Walicka/shutterstock
Fertility Case Study Update
The Fertility Case Study couples have had to use a number of the reproductive technologies mentioned so far in this lesson. As the fertility doctor for the remaining two couples—Olga and Karl and Maria and José—who have not been successful in having a positive fertilization test, you now need to discuss your patients' options with them.
To explore the multitude of reproductive technologies, complete the Read and Watch and Listen activities. Record the information in a format suitable to your learning style. Ensure that you include the pros and cons of any societal issue related to the technologies that you will be reviewing.
 Read
Read
Begin your understanding of reproductive technologies by reading pages 529 to 534 of your textbook. You may also want to read the short section about the diagnosis of genetic disorders in the fetus on pages 658 and 659.
 Watch and Listen
Watch and Listen
As with any technology, advances in reproductive technologies are made quickly. Some of the information in the multimedia pieces you are about to view may not be the most up to date technologies. However, most of the information is still correct and relevant and will therefore help you to better understand some of the technologies. These videos outline the development of fetal systems during each trimester and identify the hormones and genetic factors involved in regulating fetal development. The mechanism for exchanging nutrients and wastes between the mother and fetus, and a description of the environmental influences such as alcohol and drugs are also discussed.
As review, you may choose to watch the entire video “Reproductive Technologies and Sexually Transmitted Disease: Eggs, Embryos, and Ethics”; however, concentrate on the following segments:
- “Bio Probe: Assisted Reproductive Technologies”
- “Fertility Treatments”
- “Bio Discovery: Ethics of Reproductive Technology”
- “Concept Map: Treating Infertility”
Also view “Hormonal Controls and Conception: A Reproduction Rhapsody.” This video also provides a good review of the concepts of this unit. You may watch the entire video, or you may concentrate on the section “Bio Discovery: Contraceptive Methods and Devices” and continue viewing to the end of the video. You may be required to enter a username and password in order to view the video. Contact your teacher for this information.
The "Ultrasound: How Does it Work?" gizmo outlines the development of fetal systems during each trimester and identifies the hormones and genetic factors involved in regulating fetal development. It also shows how ultrasound is used to study development, illustrates the mechanism for exchanging nutrients and wastes between the mother and fetus, and describes the environmental influences such as alcohol and drugs.
 Try This
Try This
TR 1. Work by yourself or in a group to complete "Thought Lab 15.2: Evaluating Reproductive Technologies: Safety and Effectiveness" on page 533 of the textbook.
You may choose to consult with other students and your teacher to exchange additional information and to summarize findings for all the technologies investigated. Consult with your teacher for the answers to this lab.
 Discuss
Discuss
Through your discussion board, discuss one, some, or all of the following questions.
D 1. What is your opinion about the use of technology to help mother and child bond?
D 2. How do you think North American society has been affected by the use of reproductive technologies?
D 3. A 3-D ultrasound produces a three-dimensional image of the fetus, generally in a still picture format. A 4-D ultrasound is like viewing a video tape of the fetus inside the womb. Do you think that a mother would be more inclined to practise a healthy lifestyle if she could view her baby in a 4-D ultrasound?
D 4. Can you think of a new or different type of reproductive technology that could improve any component of human reproduction?
D 5. What are the advantages and disadvantages to society when social support is provided to single parents who might need support to raise their children?
D 6. Should health care plans help compensate couples for costs related to adoption and in vitro fertilization?
 Self-Check
Self-Check
SC 1. See how well you understand reproductive technologies by completing questions 33 to 36 on pages 530 and 532 of the textbook.
 Self-Check Answers
Self-Check Answers
SC 1.
Textbook questions, pages 530 and 532
- Students should cite any two of the following reasons for male infertility: obstructions in the ductus deferens or epididymis; low sperm count; high proportion of abnormal or non-viable sperm; inability to achieve an erection or ejaculation; smoking; alcohol use, overheated testicles. Treatments can include: healthier lifestyle (cutting back on smoking, alcohol, wearing looser clothing); artificial insemination; in vitro fertilization; use of a sperm bank.
- Students should cite any two of the following reasons for female infertility: blocked oviducts; failure to ovulate; endometriosis; damaged eggs. Treatments can include artificial insemination; in vitro fertilization; surrogate mothers; superovulation.
- The most effective method to avoid conceiving a child is to practice abstinence. It not only prevents pregnancy, it also helps to minimize the risk of STIs.
- The technology that does the best job of preventing conception and protecting against the transmission of STIs is a combination of condoms (a physical barrier) and chemical barriers (spermicides in the form of jellies, foams, or creams).
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), TRM 530–532. Reproduced by permission.
1.18. Page 3
Module 4—From Fertilization to Birth
 Reflect and Connect
Reflect and Connect
The opinions surrounding reproductive technologies are based on individual experiences and exposure to the issue in question. In North America, no restraints are placed on families in regard to the number of children they can have. In 1979, China implemented a one-child policy to deal with the country’s growing population and the resulting social and environmental problems. The Chinese government reviewed this policy in February of 2008, at which time it was decided to maintain the implementation of the one-child policy for another ten years.
Write a reflection of how this policy would impact your family (present and future) and society if it were implemented in Alberta. How could this policy be enforced or adhered to? What are the reproductive technology implications that would result from such a policy? Should families be taxed based on the number of children they have? Would this be based on the assumption that the impact of a family with more children would be greater on society and the environment than a family with fewer children? Submit your reflection to your teacher for feedback.
 Reflect on the Big Picture
Reflect on the Big Picture

© Monkey Business Images/shutterstock
Fertility Case Study Update
Every individual and couple needs to make the final decision about the extent to which they will use reproductive technology. Not only are the ethical and moral issues important to consider, but the cost of treatments, like in vitro fertilization, can be approximately $10 000/treatment, thereby making this option one that is not affordable for all couples or individuals.
The two remaining couples from the Fertility Case Study, who have not been able to conceive, have each made a decision about the route they wish to follow to have a family. Because Karl and Olga already have two children in their family from Karl’s first marriage, they have decided to investigate extending their family through reproductive technologies or through adoption.
Maria and José decided to use reproductive technologies to help them become pregnant. Maria is now pregnant with twins.
 Going Beyond
Going Beyond
Reproductive technologies always bring with them controversy—ethical and moral issues related to their use. What do you believe are the ethical and moral issues relating to the use of reproductive technologies? What have governments in Canada done to deal with the concerns about the use of reproductive technologies? First, see if you can find any government legislation or policies in Canada, or any other country, that deal with the use of reproductive technologies. Then, do a comparison of those you find.
 Module 4: Lesson 4 Assignment
Module 4: Lesson 4 Assignment
There is no assignment for this lesson.
You may wish to consult with your teacher about which questions on page 534 of the textbook would provide you with a good review of this lesson. Your teacher can provide feedback for your responses.
1.19. Page 4
Module 4—From Fertilization to Birth
 Lesson Summary
Lesson Summary
The following focusing question was addressed in this lesson:
- What technologies are used to assist fertilization, to monitor development, and to facilitate parturition?
Throughout history humans have tried to control their reproductive potential. Reproductive technologies first began as attempts to prevent pregnancy, and have now evolved into advanced contraceptive methods and into extremely advanced technologies used to enhance reproductive success. Reproductive technologies have also advanced to allow the monitoring of embryonic and fetal development, and scientists and doctors have even developed the technology and skill to make fetal surgery possible.
Developed countries have also made advances in technologies that assist in parturition. These advances in technology have not been seen in developing countries where women often die in childbirth.
The development and use of reproductive technologies have come a long way. However, there will always be an ethical and moral debate about the practice and use of reproductive technologies.
Lesson Glossary
abstinence: not having sexual intercourse; is often practiced in order to prevent pregnancies and decrease the risk of trasnmitting or receiving STIs
amniocentesis: a fetal diagnostic technique done by inserting a syringe through the mother’s abdominal and uterine walls to extract a sample of amniotic fluid, which contains sloughed-off embryonic cells; used to karyotype the embryo and diagnose chromosome non-disjunctions, such as Down’s syndrome
artificial insemination: a procedure in which semen from a donor is inserted by syringe into the vagina of a receptive female; used in the case of male infertility
barriers: any chemical or physical device that stops sperm from meeting the egg
Examples of barriers include spermicides and condoms.
chorionic villi sampling (CVS): a fetal diagnostic technique done by pinching off a small sample of chorionic villus; sample is obtained vaginally
Because chorion cells are embryonic, cells can be karyotyped to diagnose chromosomal non-disjunctions, such as Down’s syndrome.
contraceptive hormone treatment: birth control pills, birth control patches, and injections using estrogen-progesterone combinations to suppress ovulation, thus preventing pregnancy
cordiocentesis: the process of sampling fetal blood from the umbilical cord to test for the possibility of infection or blood disease
family planning: natural birth control that consists of avoiding sex during the fertile period around ovulation; can be tested for by a small increase in core temperature; not very effective
fetal surgery: surgery to correct congenital defects while the fetus is still in the uterus
home pregnancy test: a urine test that indicates if HCG is present in the urine
HCG is only produced by a chorion, so it indicates pregnancy.
in vitro fertilization (IVF): a process in which multiple eggs harvested from a female are combined with sperm in the lab, and the resulting embryo is implanted into the female; used in cases of female infertility
ovulation test kits: home kits that test the urine for a surge in LH, which indicates that ovulation will occur shortly; used to time intercourse to maximize the chances of conceiving
reproductive technology: any application of human intelligence that increases or decreases reproductive potential
superovulation: hormones similar to FSH are prescribed to stimulate the ovary to produce eggs more consistently
Conception may be natural or eggs may be harvested from the ovary to be used in IVF.
surrogate motherhood: the process by which an embryo is inserted into the uterus of a woman who will carry the fetus to term, then return the baby to the biological parents; used when a woman cannot undergo pregnancy
tubal ligation: permanent female sterilization in which the Fallopian tubes (oviducts) are cut and sealed to prevent further ova from passing from the ovaries to the site of fertilization
ultrasonography: fetal diagnostic technique by which high-frequency sound waves are bounced off the fetus, providing images of internal and external fetal structures
vasectomy: permanent male sterilization in which the ductus deferens are cut and sealed to prevent sperm from passing from the epididymis into the semen
1.20. Module Summary/Assessment
Module 4—From Fertilization to Birth
 Module Summary
Module Summary
In this module you were asked the following inquiry question:
- From fertilization to birth, how is cell differentiation and development regulated by genetic, endocrine, and environmental factors?
From the moment of fertilization through embryonic and fetal development, an amazing transformation occurs in a prenatal organism. The speed at which the changes take place from a single-celled organism to a multicellular organism that is capable of surviving on its own is truly incredible. Once fertilization takes place, the development of the embryo begins. Different layers begin to form, with each of these layers giving rise to more specialized types of tissues and functions. Various membranes support the embryo and help form the placenta which nourishes and supports the fetus.
The development and maintenance of the offspring in utero is controlled by hormones produced by various supporting structures. Once all the major organs and systems are in place, a tremendous amount of growth and maturation of the systems happens. Any time during prenatal development, genetic, hormonal, and environmental factors can affect the developing offspring. However, it is the first three months, specifically the first eight weeks, of development that are most critical.
Hormones initiate the birthing process, resulting in the forceful uterine contractions that expel the fetus and placenta. Once birth has occurred, hormones trigger lactation, or the delivery of milk from the mammary glands.
A myriad of technologies have been developed to control human sexual reproduction. There are technologies that can enhance or reduce reproduction potential, monitor development, and assist in the birthing process. The use of reproductive technology often results in controversy over social and ethical issues.
In this module, the following focusing questions were addressed:
- What are the sequences of events and hormone controls that occur throughout fertilization and embryonic development?
- What major tissues and organs arise from the ectoderm, mesoderm, and endoderm?
- How are twins formed?
- What are the major events of each trimester?
- What is the significance of the first trimester?
- What is the significance of the effects of teratogens on embryonic and fetal development?
- What triggers the birthing process, and what are its stages?
- What controls lactation?
- What technologies are used to assist fertilization, to monitor development, and to facilitate parturition?
To review and summarize the concepts of Module 4, you may wish to complete the Module 4 Concept Organizer. You may have already saved a copy of this document when you first encountered it in the Big Picture section, or you may download it now. It is an outline of the lessons that contains the focusing questions for Module 1. Use the focusing questions to fill in this concept organizer with the ideas that you mastered in each lesson. You can use keywords, point form, or any amount of detail that meets your needs. You may choose to work from the file on your computer, print the document and work from the paper copy, or copy the outline onto a large sheet of poster paper. This is a great tool to review and use for study purposes.
Before you begin the Module Assessment, you may want to complete some of the questions on pages 536 and 537 in your textbook as a review. Review questions for all of Unit B can be found on pages 540 to 543 in the textbook. Your teacher can suggest which questions would be best for you to complete and provide you with feedback about your responses.
Module Assessment
Dividing the prenatal development and parturition events into different periods or stages is a way to gauge normal progress. It is important to remember that not all pregnancies and labours follow these exact time frames. However, you do need to understand the overall progress and relative time periods described. Many factors and technologies can prevent or assist in prenatal development and observation.
Work with a partner or small group that has been approved by your teacher to show your understanding of the content in Module 4 by planning, designing, and creating a multimedia presentation that addresses all of the following points.
- Describe all major events and components of prenatal development, from fertilization to the end of the fetal development period, including hormonal control and significant developmental events happening in each trimester.
- State and describe three factors that affect embryonic and fetal development. The three factors must include one genetic factor, one hormonal factor, and one environmental factor. For each of these three factors, state how the embryonic germ tissue will be affected and how this may or may not affect fetal development.
- Examine parturition events and explain the hormonal and neural components that cause the onset of labour through to the end of the placental stage.
- Describe the events that need to happen for successful lactation to occur.
- Examine reproductive technologies by describing at least one technology that enhances reproductive potential, at least one technology that reduces reproductive potential, and one technology that is used to monitor embryonic or fetal development. Discuss any societal, cultural, environmental, ethical, or economic considerations in the use of these technologies.
The following rubric will help you prepare your answer. Remember that complete, clearly explained work is necessary in this type of question. Each question is worth 5 marks, making your presentation worth a total of 25 marks.
1.21. Module Glossary
Module 4—From Fertilization to Birth
Module Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
allantois: extra-embryonic membrane that forms the foundation for the umbilical cord, which connects the fetus with the placenta
amnion: extra-embryonic membrane that is a closed, fluid-filled sac surrounding the fetus; protects the fetus from impact and temperature change
blastocyst: embryonic stage that results when the morula hollows out; the outer layer is the trophoblast and becomes the chorion; the inner cell mass becomes the embryonic disc
Caesarean section (C-section): a surgical procedure in which the fetus is removed from the abdomen through an incision; used when vaginal birth is difficult or impossible
chorion: outermost layer of the embryo; develops from the trophoblast layer of the blastocyst; will form the fetal blood pool of the placenta
cleavage: cell division in which the zygote divides into smaller, identical cells, called blastomeres, without increasing the total size of the cell mass
colostrum: a rich, yellow secretion from the mammary glands that occurs for two to three days prior to the first secretion of milk; contains mother’s antibodies to protect the newborn from disease
contractions: the rythmic shortening of the muscles of the uterus to expel the fetus
differentiation: the turning on and off of genes in a cell; results in specialized cell functions
dilation: the opening of the cervix to allow passage of the baby
dilation stage: the stretching and opening of the cervix to 10 cm to allow passage of the fetus during expulsion
dizygotic twins: twins that form when two eggs are fertilized by two sperms; also known as fraternal twins; may be of different sexes
ectoderm: germ layer that forms hair, nervous system, and skin
ectopic pregnancy: occurs when fertilization and implantation take place in the oviduct
embryo: the organism in the stages of development from the time the zygote begins cleavage until nine weeks of gestation, when the embryo becomes a fetus
endoderm: germ layer that forms gut lining, pancreas, and liver
expulsion stage: the stage in which the smooth muscle walls of the uterus contract in rhythmic cycles to deliver the fetus from the vagina
extra-embryonic membranes: membranes surrounding the embryo, and later the fetus, that support its development in different ways; include the allantois, amnion, chorion, and yolk sac
fertilization: the fusing of a sperm nucleus with an egg nucleus to form a zygote; occurs in the oviduct
fetal alcohol spectrum disorder: a permanent syndrome of birth defects caused by maternal intake of alcohol during pregnancy; includes disorders of growth, behaviour, and cognitive abilities
fetus: the organism in the stages of development from nine weeks until birth
folic acid (folate): Vitamin B9; ingestion prior to and during pregnancy prevents neural tube defects, such as spina bifida
gastrulation: the folding and differentiation of the embryonic disc into three germ layers, forming the embryonic stage called the gastrula
human chorionic gonadotropin (HCG): hormone released from the chorion after implantation; directs corpus luteum to continue making estrogen/progesterone, thereby maintaining the endometrium and preventing menstruation
implantation: burrowing of the blastocyst into the wall of the endometrium of the uterus
lactation: the production and secretion of milk from the breast; also known as “nursing”
mesoderm: germ layer that forms muscle, bone, and muscular organs
monozygotic twins: identical twins formed when the embryonic mass produced by the union of one egg and one sperm splits into two separate, identical masses; are of the same sex
morphogenesis: the development of body organs and structures; begins with gastrulation
morula: embryonic stage of a solid ball of identical cells that results from cleavage of the zygote
neurulation: the process of forming the embryo's neural tube, which will develop into the brain and spinal cord
parturition: childbirth or labour
parturition: the process of labour and delivery, which is divided into dilation, expulsion, and placental stages
placenta: embedded in the endometrium; provides a location where nutrients, gases, and wastes can be exchanged between fetal and maternal blood pools
placental stage: the stage in which further uterine contractions push the placenta out of body through the vagina; also known as delivery of the afterbirth
prenatal: before birth
primary germ layers: three layers formed during gastrulation—endoderm, mesoderm, and ectoderm
prostaglandins: a group of hormones that contribute to parturition by thinning the cervix and increasing contraction of the uterus
sucking reflex: an instinctive sucking action by a newborn that stimulates oxytocin secretion in the mother; results in release of milk from the mammary glands into the milk ducts of the breast
teratogen: a substance or other factor that can cause developmental abnormalities during fetal development; e.g., chemicals, viruses, or radiation
trimester: one-third of the gestational period
There are three trimesters of pregnancy.
umbilical cord: tube of blood vessels that connects the fetus to the placenta; for exchange of nutrients, gases, and wastes
vernix: a cheesy, oily substance covering the fetus; has antibacterial properties
yolk sac: extra-embryonic membrane that produces first blood cells
zygote: the one-celled product of egg and sperm fusion; also known as the fertilized egg