Module 3
| Site: | MoodleHUB.ca 🍁 |
| Course: | Biology 30 SS |
| Book: | Module 3 |
| Printed by: | Guest user |
| Date: | Friday, 19 December 2025, 4:19 AM |
Description
Created by IMSreader
Table of contents
- 1. Module 3
- 1.1. Big Picture
- 1.2. In this Module
- 1.3. Lesson 1
- 1.4. Page 2
- 1.5. Page 3
- 1.6. Page 4
- 1.7. Lesson 2
- 1.8. Page 2
- 1.9. Page 3
- 1.10. Page 4
- 1.11. Lesson 3
- 1.12. Page 2
- 1.13. Page 3
- 1.14. Page 4
- 1.15. Page 5
- 1.16. Lesson 4
- 1.17. Page 2
- 1.18. Page 3
- 1.19. Page 4
- 1.20. Lesson 5
- 1.21. Page 2
- 1.22. Page 3
- 1.23. Page 4
- 1.24. Lesson 6
- 1.25. Page 2
- 1.26. Page 3
- 1.27. Page 4
- 1.28. Lesson 7
- 1.29. Page 2
- 1.30. Page 3
- 1.31. Page 4
- 1.32. Lesson 8
- 1.33. Page 2
- 1.34. Page 3
- 1.35. Page 4
- 1.36. Lesson 9
- 1.37. Page 2
- 1.38. Page 3
- 1.39. Page 4
- 1.40. Module Summary/Assessment
- 1.41. Module Glossary
1. Module 3
Module 3—The Male and Female Reproductive Systems
Introduction
© 2009 Jupiterimages Corporation
During the wild ride of puberty, everybody gains some personal knowledge about the unique features in both the human male and human female body. These structures are specialized to perform unique functions to ensure production of the next generation and survival of the human species through sexual reproduction. You may already think that you know the differences between the male and female reproductive systems, but, in this module, you will discover many more structures that are unique and suited to perform specialized functions. You will also study how sexually transmitted infections can affect the reproductive systems and a developing fetus.
By examining the human reproductive systems, you will gain perspective on how the human species has managed to increase its population size on a constantly changing planet. Lessons 1 to 5 of this module will examine the structures and functions of the human reproductive systems and the implications of sexually transmitted infections on fertility. Lessons 6 to 9 will examine how hormonal regulation of the male and female reproductive systems controls the normal development and maturation of gender. You will study how the hormone feedback system in males initiates puberty, maintains a constant level of function through the reproductive years, and causes change in the aging process. In the case of females, you will examine the detailed hormonal control of the monthly menstrual cycle, the consequences to the cycle depending on whether or not fertilization has occurred, and the hormonal action that results in menopause.
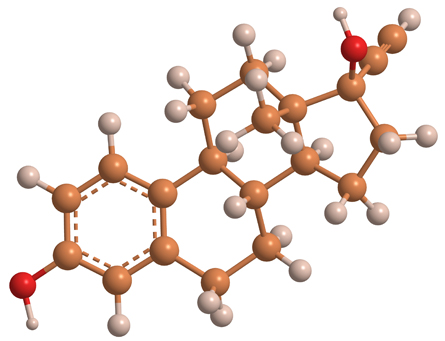
Male and female hormones are found in each gender, but in very different amounts. It is estimated that during the reproductive years men produce between 6 to 8 mg of testosterone daily, but women produce only about 0.5 mg daily. Male hormones are produced at a steady rate and do not fluctuate as cyclically as do female hormones, specifically when considering the menstrual cycle. Sex hormone distribution is controlled by negative feedback systems that maintain the appropriate amounts of hormones for sexual maturation and function. As both men and women go through the aging process, there is a reduction in the quantities of sex hormones produced.
© Natalia Karpova/shutterstock
The Module 3 Assessment will be divided into two parts. The first part will evaluate the reproductive systems and the second part will evaluate hormone control of the reproductive systems.
In addition to the Module Assessment, you will continue to collect information about the three couples struggling with infertility for the Unit Assessment.
1.1. Big Picture
Module 3—The Male and Female Reproductive Systems
 Big Picture
Big Picture
© Image courtesy of BigStockPhotos.com
As a young adult heading into your reproductive years, you are not often asked if you are planning to propagate your species. However, having a baby definitely contributes to the continuation of the human species by adding one more person to the population of the world.
You may, or may not, have considered whether your future will include your own children. That is a personal decision. When you do consider your future, you may be faced with questions such as the following:
- Do you want to have children? Why or why not? How many?
- At what age do you want to start your family?
-
Are there decisions or medical conditions that may impact your ability to conceive a child?
Some sexually transmitted infections and childhood illnesses can cause fertility problems later on in life. Diseases, such as the mumps, can cause infertility, but children who were immunized against the mumps will avoid this complication.
As a young adult, it is important to look into the future to see the consequences of choices you are making today. Although you cannot change the past, being informed can help you make better choices today and in the future.
If you suffer problems with fertility, this will make your personal choices about having a family more difficult. It may potentially also affect your role in the continuation of the human species.
In this module, lessons 1 to 5 focus on the male and female reproductive systems, and lessons 5 to 9 focus on reproductive hormones.
In Lessons 1 to 5 of this module you will explore the following focusing questions:
-
What are the structures and functions of the male and female reproductive systems?
-
What are the functional units of the male and female reproductive systems?
-
How are the functional egg and sperm supported and nourished through their development?
-
What genetic factors and hormones influence the formation of the gonads and reproductive organs in the male and female embryo and fetus?
-
How can sexually transmitted infections interfere with fertility and reproduction?
- How do social, cultural, environmental, ethical, and economic perspectives apply to decisions regarding the use of any scientific or technological developments related to human reproduction?
You have learned how gender is determined at conception and begins formation in the uterus. The remainder of Module 3 will examine the continuation of gender development throughout and after puberty.
In Lessons 6 to 9 you will explore the following focusing questions:
-
What are the male and female reproductive hormones?
-
How do hormones maintain homeostasis in the male and female reproductive systems?
-
What roles do male and female hormones play in regulating primary and secondary sex characteristics?
-
What are the physiological events of menstruation?
-
Which hormones dominate each phase of the menstrual cycle?
-
When does menstruation naturally begin and end?
-
What are the mechanisms of chemically based female and male birth control?
You have been introduced to the focusing questions for this module. Each lesson will restate these focusing questions to guide your study. To help you organize the concepts of this module, and to provide you with a potential aid for review, you may choose to download the Module 3 Concept Organizer. Fill in this concept organizer with the ideas you master as you work through each lesson, or prepare the organizer when you have completed Module 3. You can use keywords, point form, or any amount of detail that meets your needs. You may choose to work from the file on your computer, print the document and work from the paper copy, or copy the outline onto a large sheet of poster paper. After you have prepared your concept organizer, you may wish to check your work with the concept organizer provided in the Module Summary. The concept organizer provided outlines some of the key topics that you should include in each lesson of your concept organizer. This is a great tool to review and use for study purposes, but using this organizer is completely your choice.
In the Module Assessment for Module 3, you will complete evaluations of the reproductive systems and the hormonal control of them. In each lesson of Module 3, you will consider how that lesson’s topic could be related to fertility problems. You will complete some work towards the Module Assessment in each lesson. For more details about the Module Assessment and the evaluation criteria, visit the Module Summary and Assessment section.
1.2. In this Module
Module 3—The Male and Female Reproductive Systems
In This Module
Inquiry Questions:
-
What are the structures of the male and female reproductive systems, and how do these structures function to ensure the survival of the human species through reproduction?
-
How is the homeostasis of reproduction maintained by hormones in males and females?
There are nine lessons in Module 3.
Most of the lessons are designed to take the student 80 minutes to complete; however, some lessons may take longer because of the significance of the concept being covered in the lesson. The suggested lesson times do not include the time needed to complete such activities as “Try This,” “Watch and Listen,” assignments, practice questions, review, or research.
This module corresponds to Chapter 14, or pages 472 to 505, in your textbook. Before you begin your study of Lessons 1 to 9, you may wish to read Chapter 14 for an overview. As you begin each lesson, you may wish to read the relevant sections of the chapter in the textbook.
Lesson 1—the Human Male Reproductive System
In this lesson you will identify the male reproductive structures and describe their functions.
You will consider the following focusing questions:
-
What are the essential structures and functions of the male reproductive system?
-
What is the functional unit of reproduction for the male system?
Lesson 2—the Human Female Reproductive System
In this lesson you will identify the female reproductive structures and describe their functions.
You will consider the following focusing questions:
-
What are the essential structures and functions of the female reproductive system?
-
What is the functional unit of reproduction for the female system?
Lesson 3—Sperm and Egg Development
In this lesson you will distinguish sperm and egg from their supporting structures by observing images of the ovaries and testes.
You will consider the following focusing question:
- How do sperm and eggs develop into functional gametes?
Lesson 4—Chromosome and Hormone Influence
In this lesson you will learn how the sex of an embryo is determined.
You will consider the following focusing questions:
-
What are the roles of the X and Y chromosomes?
-
What hormones do they cause to be produced?
Lesson 5—Sexually Transmitted Infections and Fertility
In this lesson you will examine how sexually transmitted infections present risk to reproduction by interfering with the passage of sperm and egg, as well as how STIs create implications for a fetus.
You will consider the following focusing questions:
-
How do STIs compromise structural fertility?
-
How does cancer affect fertility?
Lesson 6—Male Hormones
In this lesson you will be learn to identify male sex hormones and their effect on the primary and secondary sex characteristics. You will learn how aging influences the male reproductive system.
You will consider the following focusing questions:
-
What are the male reproductive hormones?
-
How do hormones maintain homeostasis in the male reproductive system?
-
What role do the male hormones play in regulating the primary and secondary sex characteristics?
Lesson 7—Female Hormones
In this lesson you will learn to identify female sex hormones and their effect on the primary and secondary sex characteristics. You will learn how aging influences the female reproductive system.
You will consider the following focusing questions:
-
What are the female reproductive hormones?
-
How do hormones maintain homeostasis in the female reproductive system?
-
What role do the female hormones play in regulating primary and secondary sex characteristics?
Lesson 8—Phases of the Menstruation
In this lesson you will be able to identify when menstruation naturally begins and ends, as well as the different cycles and stages of menstruation. You will be able to identify the hormones that control specific events that occur throughout menstruation.
You will consider the following focusing questions:
-
What are the physiological events of menstruation?
-
What hormone(s) controls the specific events of menstruation?
-
When does menstruation naturally begin and end?
Lesson 9—Medical Use of Reproductive Hormones
In this lesson you will learn how medical technology helps in controlling reproductive hormones.
You will consider the following focusing question:
-
What are various medical technologies and what are their effects on reproductive hormones?
1.3. Lesson 1
Module 3:The Male and Female Reproductive Systems
Lesson 1—the Human Male Reproductive System
 Get Focused
Get Focused
Choices you make in your life are not always yours alone. When you were a young child, your parents and loved ones made many important choices for you. One of the choices they made was to decide whether or not you should be immunized against certain diseases.
You may remember the concept of antibody-mediated immunity from Biology 20. The body forms antibodies (proteins) to recognize, neutralize, and destroy foreign substances. In childhood immunization programs, children are given vaccines designed to stimulate the body’s defense mechanism into fighting off certain contagious diseases. If allowed to develop, some of these contagious diseases can have severe consequences to reproductive health. Do you know what immunizations you received as a child?

CDC/NIP/ Barbara Rice
Tim’s parents decided not to immunize him with the MMR (mumps, measles, and rubella) vaccine when he was a child. At age nineteen,Tim developed a severe case of mumps. The mumps led to orchitis—very painful swelling of the testicles. Orchitis affects one in five adult men and its symptoms can lead to infertility. This could be distressing to Tim later in life. Orchitis could cause so much damage to his reproductive structures and their normal functions that Tim may not be able to father children. You can learn more about Tim’s condition using the term “orchitis” in an Internet search.
Infertility is on the rise in North America. If infertility rises significantly at a global level, the continuity of the human species could be disrupted. Some couples are infertile because of structural or functional issues with one partner’s reproductive system.
In Lesson 1 you will investigate the male reproductive system and many issues that affect male fertility. You will investigate the following focusing questions:
-
What are the main structures and functions of the male reproductive system?
-
How do these structures support continuity of the human species?
-
What is the functional unit of the male reproductive system?
infertility: the inability to reproduce
testicles: a pair of male gonads producing sperm and testosterone; also called testes
fertility: the ability to produce gametes and reproduce
 Module 3: Lesson 1 Assignment
Module 3: Lesson 1 Assignment
Download a copy of the Module 3: Lesson 1 Assignment to your computer now. You will receive further instructions about how to complete this assignment later in the lesson.
The other questions in this lesson are not marked by the teacher; however, you should still answer these questions. The Self-Check and Try This questions are placed in this lesson to help you review important information and build key concepts that may be applied in future lessons.
After a discussion with your teacher, you must decide what to do with the questions that are not part of your assignment. For example, you may decide to submit to your teacher the responses to Try This questions that are not marked. You should record the answers to all the questions in this lesson and place those answers in your course folder.
During this lesson you will begin the Unit B Assessment project, “A Fertility Case Study.” In addition to your lesson work, store any notes about the infertile couples you learn about in your course folder for your teacher’s feedback.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities and your summary notes, file everything in your course folder to reference when you are preparing for exams.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.4. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
Do either the Read or the Watch and Listen activity first, but complete both sections. The Read and Watch and Listen activities will primarily introduce you to the major structures of the male reproductive system and their functions; however, the video includes much more information about causes of infertility and medical technologies. The information presented in these two activities is useful throughout Unit B and in the unit assessment.
 Read
Read
Your own reproductive health is important to you, but it may also be important to your future partner. Therefore, it is important that both males and females understand the structure (anatomy) and function (physiology) of the male reproductive system, including its primary reproductive organs, ducts, and accessory glands. Read pages 478 to 481 in the textbook, up to “Structures and Functions of the Female Reproductive System.” Summarize what you read by making notes, completing a chart or table similar to “Figure 14.2” on page 481, or recording the information according to your learning style. You must include a labelled diagram of the male reproductive system in your notes. Save your work in your course folder. Make sure that your work includes information on gonad, sperm, sex hormone, primary and secondary sex characteristics, gamete, testes, scrotum, seminiferous tubules, Sertoli cells, epididymis, ductus deferens, ejaculatory duct, penis, seminal vesicle, prostate gland, Cowper’s gland, semen, urethra, and ejaculation.
gonads: sex organs that produce gametes (sperm or egg); testes in males and ovaries in females
sperm: the male gamete
In sexual reproduction, the haploid sperm contributes half the chromosomes to the zygote; the egg contributes the other half.
sex hormone: a biochemical compound controlling the development, maintenance, and function of the reproductive system and secondary sex characteristics
primary sex characteristics: structures in the male or female that are essential for reproduction
secondary sex characteristics: characteristics that distinguish male from female but are not required for reproduction
gamete: a haploid cell made during meiosis that participates in fertilization to make a zygote
testes: paired male gonads that produce sperm and secrete testosterone
scrotum: a pouch of skin located below the penis that holds the testes
seminiferous tubules: coiled, hollow tubes in the testes where sperm are produced
Sertoli cells: ‘nurse’ cells in the seminiferous tubules that assist in spermatogenesis and produce the hormone inhibin
epididymis: a cap on each testicle where sperm are matured and stored prior to ejaculation
ductus deferens: a smooth muscle tube that carries the semen from the epididymis to the penis
ejaculatory duct: a tube from the ductus deferens to the penis
penis: the copulatory organ of the male that transfers semen to the female
seminal vesicles: glands producing a fluid containing fructose, which supplies energy for use by sperm
prostate gland: a muscle-like gland secreting alkaline fluid to neutralize the acids in urine
Cowper’s gland: a gland secreting fluids to form semen
semen: the ejaculated liquid that contains sperm plus the secretions of the seminal vesicles, prostate, and Cowper’s gland
urethra: the tube leading from the bladder to the penis
The urethra may carry either urine or semen.
ejaculation: the release of semen from the penis
 Watch and Listen
Watch and Listen
Watch the video “The Male Reproductive System: Perpetuating the Species” from the beginning of the video to the end of the section “The Male Reproductive System Anatomy II” to further your understanding of the male reproductive system. The video helps you to see another view of the structures involved in the male system. Answer the questions for “The Male Reproductive System: Perpetuating the Species” as you watch the video. Save your answers in your course folder.
 Self-Check
Self-Check
Test your knowledge of the location of various structures in the male reproductive system by completing this "Male Reproductive System" drag-and-drop activity.
1.5. Page 3
Module 3—The Male and Female Reproductive Systems
 Reflect and Connect
Reflect and Connect
The Sperm Pathway and Orchitis
Think back to nineteen-year-old Tim who developed a severe case of mumps, which led to orchitis. How might orchitis affect his reproductive system? Assume that Tim is not very aware of his own reproductive system. As a friend, you will use what you have learned in this lesson to help Tim understand his reproductive system, orchitis, and the effects the condition may have on the structures and functions of the male reproductive system.
 Module 3: Lesson 1 Assignment
Module 3: Lesson 1 Assignment
There are two parts to this assignment. Answer each part through a detailed illustration or diagram, PowerPoint presentation, video, cartoon, animation, written report, podcast, or any other form approved by your teacher. You may respond through a different form for each of the two parts.
Retrieve your copy of Module 3: Lesson 1 Assignment that you saved to your computer earlier in this lesson. Complete questions 1 and 2. Save your completed assignment in your course folder. You will receive instructions later in this lesson about when to submit the assignment to your teacher.
 Discuss
Discuss
Write a paragraph to respond to two of the questions below (one paragraph per question). Post your responses to the discussion area for your class. Read the responses of at least two other students. If possible, discuss the responses amongst yourselves.
-
What does being male mean to you? Is it just about anatomy and hormones?
-
What are some of the threats to a healthy male reproductive system? Which threats can you control? How can you deal with the threats that are out of your control?
-
What are the implications of a lower sperm count in North American men?
-
What are the implications of a low or reduced fertility rate in North America?
 Reflect on the Big Picture
Reflect on the Big Picture
You now know the structures and functions of the male reproductive system. You may also have identified that the sperm cell is the functional unit of the male reproductive system.
Recall the three couples with fertility problems described in the introduction to Unit B:
- Couple 1—John and Jane
- Couple 2—José and Maria
- Couple 3—Karl and Olga
From the information given about the couples and the knowledge you have gained so far in Unit B, can you identify any specific problems with any of these couples that could help solve their fertility problems? Are there additional questions you could ask to help identify other problems? You may need to read through the couples’ information again in the introduction to “A Fertility Case Study.” Make notes about your conclusions or assumptions and place them in your course folder. Remember that information and questions about the couples’ fertility issues will be referred to throughout Unit B and will be part of the Unit B Assessment.
 Going Beyond
Going Beyond
Build on what you know about the male reproductive system by finding out what can be done if something goes wrong with its structures or functions. You can do further research on the main male reproductive structures to find a dysfunction that can occur with each one, and a treatment to overcome each dysfunction.
 Module 3: Lesson 1 Assignment
Module 3: Lesson 1 Assignment
Submit your completed Module 3: Lesson 1 Assignment to your teacher for assessment.
1.6. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In Lesson 1 you investigated the following focusing questions:
-
What are the main structures and functions of the male reproductive system?
-
How do these structures support continuity of the human species?
-
What is the functional unit of the male reproductive system?
The male reproductive system is designed to produce and release large numbers of sperm. The gametes (sperm) are produced within the seminiferous tubules in the gonads (testes), where the temperature for proper sperm development is controlled by the scrotum. There the developing sperm are supported by the Sertoli cells and are transferred to the epididymis to be matured and stored.
During ejaculation, the ductus deferens helps transfer the sperm from the testes to the urethra, picking up the semen and seminal fluids on the way. The seminal fluids help the sperm by providing sugar for energy, alkalinity to neutralize urine and vaginal acids, and a medium for motility. Semen leaves the male body through the penis. The male reproductive system and sperm structure allow for sperm to be deposited into the female and to move through the female reproductive system.
Childhood illnesses, sexually transmitted infections, structural problems, and environmental and societal factors can all interrupt the function of the male reproductive system. The end result of sexual reproduction is the formation of a fertilized egg that contributes to variation and continuation of the human species.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
Cowper’s gland: a gland secreting fluids to form semen
ductus deferens: a smooth muscle tube that carries the semen from the epididymis to the penis
ejaculation: the release of semen from the penis
ejaculatory duct: a tube from the ductus deferens to the penis
epididymis: a cap on each testicle where sperm are matured and stored prior to ejaculation
fertility: the ability to produce gametes and reproduce
gamete: a haploid cell made during meiosis that participates in fertilization to make a zygote
gonads: sex organs that produce gametes (sperm or egg); testes in males and ovaries in females
infertility: the inability to reproduce
penis: the copulatory organ of the male that transfers semen to the female
primary sex characteristics: structures in the male or female that are essential for reproduction
prostate gland: a muscle-like gland secreting alkaline fluid to neutralize the acids in urine
scrotum: a pouch of skin located below the penis that holds the testes
secondary sex characteristics: characteristics that distinguish male from female but are not required for reproduction
semen: the ejaculated liquid that contains sperm plus the secretions of the seminal vesicles, prostate, and Cowper’s gland
seminal vesicles: glands producing a fluid containing fructose, which supplies energy for use by sperm
seminiferous tubules: coiled, hollow tubes in the testes where sperm are produced
Sertoli cells: ‘nurse’ cells in the seminiferous tubules that assist in spermatogenesis and produce the hormone inhibin
sex hormone: a biochemical compound controlling the development, maintenance, and function of the reproductive system and secondary sex characteristics
sperm: the male gamete
In sexual reproduction, the haploid sperm contributes half the chromosomes to the zygote; the egg contributes the other half.
testes: paired male gonads that produce sperm and secrete testosterone
testicles: a pair of male gonads producing sperm and testosterone; also called testes
urethra: the tube leading from the bladder to the penis
The urethra may carry either urine or semen.
1.7. Lesson 2
Module 3—The Male and Female Reproductive Systems
Lesson 2—the Human Female Reproductive System
 Get Focused
Get Focused
© Laurence Gough/shutterstock
In Lesson 1 you learned about the important role the male reproductive system plays in the continuation of the human species. While he is a vital contributor to reproduction, the male cannot reproduce by himself. To understand how the human species is perpetuated, it is vital to understand the other half of the equation—the structures and functions of the female reproductive system. It is the female reproductive system that forms, develops, and delivers a new human organism to functional independence as a newborn baby. This is a complex process that requires all parts of the female system to work in synchronicity.
During puberty, the female reproductive system undergoes many changes, such as menarche, the start of menstruation. Menstrual cramps, mild to severe pressure or pain experienced in the abdominal and pelvic areas, are an unpleasant symptom of menstruation for many young women.
menarche: a female’s first menstrual cycle
menstruation: the monthly shedding of the endometrial lining
dysmenorrhea: severe menstrual cramps
Estimates suggest that 50% of women suffer from cramping, with up to 15% of these women defining their menstrual cramps as severe. The medical term for painful menstrual cramps is dysmenorrhea. Women who have chronic cramping may or may not have trouble with fertility.
In addition to the pain experienced in the abdomen and pelvis, menstrual cramps can be associated with one or more of the following ailments: headaches, nausea, vomiting, constipation, or diarrhea. You may have seen advertisements for over-the-counter medication to help alleviate some of these symptoms.

© 2008 Jupiterimages Corporation
Update: A Fertility Case Study
Maria, from the second couple introduced in the Unit B “A Fertility Case Study,” suffers from dysmenorrhea. Her condition developed over eight months when she was 14 years old. By the time she was 15 years old, Maria was unable to function normally during her menstrual cycle. To manage the pain of severe cramps, Maria, with her mother’s guidance and supervision, tried several over-the-counter pain medications. These medications provided less and less pain relief as time went on.
To learn more about the female reproductive system and the different treatment options available for dysmenorrhea, Maria and her mother went to their local sexual health centre. They wanted to make sure they understood the decisions they were making and the effects those decisions would have on Maria’s long-term reproductive health. You can learn more about Maria’s condition using the term(s) “dysmenorrhea” or “severe menstrual cramps” in an Internet search.
In Lesson 2 you will investigate the female reproductive system and many issues that affect female fertility.
You will investigate the following focusing questions:
-
What are the essential structures and functions of the female reproductive system?
-
How do these structures support continuity of the human species?
-
What is the functional unit of the female reproductive system?
 Module 3: Lesson 2 Assignment
Module 3: Lesson 2 Assignment
Download a copy of the Module 3: Lesson 2 Assignment to your computer now. You will receive further instructions about how to complete this assignment later in the lesson.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
During this lesson you will continue the Unit B Assessment project, “A Fertility Case Study.” In addition to your lesson work, store any information about the infertile couples you learn about, specifically information about Sarah, in your course folder for your teacher’s feedback.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.8. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
 Read
Read
Like males, females must also maintain good sexual health. Successful reproduction is dependent on both sexes and their roles; therefore, it is important that both males and females understand the structure and function of the female reproductive system. Read textbook pages 481 to 484, beginning at “Structure and Functions of the Female Reproductive System” and ending with “Differences Between Sperm Cells and Egg Cells.” Summarize what you read by making notes, completing a chart or table similar to “Table 14.3” on page 484, or recording the information according to your learning style. You must include a labelled diagram of the female reproductive system in your notes. Ensure that you include information on ovaries, egg or ova, follicles, ovulation, fimbriae, oviduct, uterus, zygote, endometrial lining, cervix, vagina, embryo, and vulva. Save your work in your course folder.
ovaries: the paired female gonads that produce eggs and secrete progesterone and estrogen hormones
egg [ovum (singular), ova (plural), oocyte]: the female gamete that contributes half of the chromosomes to the zygote in sexual reproduction
follicles: specialized cells that surround and nurture the developing ova in the ovary and that secrete estrogen and progesterone
ovulation: the release of the mature ovum from the follicle of the ovary into the oviduct
fimbriae: finger-like projections that sweep the ovulated ovum into the oviduct
oviduct (Fallopian tube): the cilia-lined tube of smooth muscle that carries the ovulated egg from each ovary to the uterus
uterus: the reproductive organ in which embryonic and fetal development occurs
zygote (fertilized egg): a single cell produced by the fusion of the egg and sperm
endometrial lining: the lining of the uterus that is thickened monthly to allow implantation of an embryo, and is shed in menstruation if fertilization does not occur
cervix: the tightly constricted opening from the vagina into the uterus
vagina: the muscular tube that leads from the uterus to the external environment
embryo: the offspring in the period of development from the cleavage of the zygote to the ninth week, when the embryo becomes a fetus
vulva: the external female genital organs
 Try This
Try This
TR 1. Answer questions 1 through 8 on page 485 of the textbook. If you choose to answer these questions, you do not have to answer the question sheet in the Watch and Listen activity; however, ensure that you discuss your answers with your teacher.
 Watch and Listen
Watch and Listen
Watch the following segments of “The Human Female Reproductive System: A Creation of Exquisite Synchrony.” Make notes as you watch. File your notes in your course folder. You may be required to enter a username and password in order to access these videos. Contact your teacher for this information.
-
“Overview: Female Reproductive System”
-
“Bio Reports: Female Reproductive System”
-
“Ovary”
-
“External Female Genital Organs”
-
“Bio Review: Female Reproductive System”
If you chose not to answer questions 1 through 8 in the Try This activity above, answer the questions about “The Human Female Reproductive System: A Creation of Exquisite Synchrony” as you watch the video. Save your answers in your course folder.
 Try This
Try This
TR 2. Test your knowledge of the location of various structures in the female reproductive system by completing the “Female Reproductive System” drag-and-drop activity.
1.9. Page 3
Module 3—The Male and Female Reproductive Systems

© 2008 Jupiterimages Corporation
 Reflect and Connect
Reflect and Connect
Egg Pathway
Think back to Maria and her condition of dysmenorrhea. Imagine that you are a sexual health nurse who is helping Maria and her mother address Maria’s menstrual cramps. It is important for you to explain, in appropriate language, what Maria and her mother need to know to make an informed choice regarding treatment options.
 Module 3: Lesson 2 Assignment
Module 3: Lesson 2 Assignment
Retrieve your copy of Module 3: Lesson 2 Assignment that you saved to your computer earlier in this lesson. Complete questions 1 and 2 by creating detailed illustrations or diagrams, PowerPoint presentations, videos, cartoons, animations, written reports, podcasts, or any other form approved by your teacher. You may respond in a different format for each of the two questions. Save your completed assignment in your course folder. You will receive instructions later in this lesson about when to submit your assignment to your teacher.
 Discuss
Discuss
Write a paragraph to respond to two of the questions below (one paragraph per question). Post your responses to the discussion area for your class. Read the responses of at least two other students. If possible, discuss the responses amongst yourselves.
- What does being female mean to you? Is it just about anatomy and hormones?
-
What are some of the threats to a healthy female reproductive system? Which threats can you control? How can you deal with the threats that are out of your control?
-
What are the pros and cons of postponing having children to pursue other goals?
-
Can a woman who only has a left ovary and a right Fallopian tube become pregnant? Why or why not?
 Reflect on the Big Picture
Reflect on the Big Picture
Case Study Update
You now know the structures and functions of the female reproductive system. You may also have identified that the egg cell is the functional unit of the female reproductive system. Recall the three couples with fertility problems described in the introduction to Unit B.
-
Couple 1—Jane and John
-
Couple 2—Maria and José
-
Couple 3—Olga and Karl
Continue to make notes about the couples' fertility problems, specifically those of Maria. Save your notes, including conclusions or assumptions, in your course folder. Remember that information and questions about the couples’ fertility issues will be referred to throughout Unit B and will be part of the Unit B Assessment.
 Going Beyond
Going Beyond
Build on what you know about the female reproductive system by finding out what can be done if something goes wrong with its structures or functions. You can do further research on the main female reproductive structures to find a dysfunction that can occur with each one and a treatment to overcome each dysfunction.
 Module 3: Lesson 2 Assignment
Module 3: Lesson 2 Assignment
Submit your completed Module 3: Lesson 2 Assignment to your teacher for assessment.
1.10. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In Lesson 2 you investigated the following focusing questions:
-
What are the essential structures and functions of the female reproductive system?
-
How do these structures support continuity of the human species?
-
What is the functional unit of the female reproductive system?
The female reproductive system is designed to produce a very limited number of gametes. The female gonads (ovaries) produce the egg (ovum), the functional unit of reproduction for the female. An egg is further matured inside a follicle, within an ovary. Once matured, the egg, through the process of ovulation, ruptures out of the ovary. Outside of the ovary, the fimbriae pick up the egg and sweep it into the oviduct (Fallopian tube). With the help of cilia and muscle contractions in the oviduct, the egg is transported to the uterus. If a sperm fertilizes the egg in the oviduct, the resulting zygote may implant in the uterus, resulting in the development of a new human life. If a sperm does not fertilize the ovum, the ovum is transported out of the uterus during menstruation with the shedding of the endometrial lining through the cervix and vagina to the outside of the body.
Because only a limited number of gametes are produced, protection of the egg and the developing embryo is critical. Their protection is ensured by internal fertilization and development. The female reproductive system is one-half of the equation that brings a new human life into the world and contributes to the continuation of the human species.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
cervix: the tightly constricted opening from the vagina into the uterus
dysmenorrhea: severe menstrual cramps
egg [ovum (singular), ova (plural), oocyte]: the female gamete that contributes half of the chromosomes to the zygote in sexual reproduction
embryo: the offspring in the period of development from the cleavage of the zygote to the ninth week, when the embryo becomes a fetus
endometrial lining: the lining of the uterus that is thickened monthly to allow implantation of an embryo, and is shed in menstruation if fertilization does not occur
fimbriae: finger-like projections that sweep the ovulated ovum into the oviduct
follicles: specialized cells that surround and nurture the developing ova in the ovary and that secrete estrogen and progesterone
menarche: a female’s first menstrual cycle
menstruation: the monthly shedding of the endometrial lining
ovaries: the paired female gonads that produce eggs and secrete progesterone and estrogen hormones
oviduct (Fallopian tube): the cilia-lined tube of smooth muscle that carries the ovulated egg from each ovary to the uterus
ovulation: the release of the mature ovum from the follicle of the ovary into the oviduct
uterus: the reproductive organ in which embryonic and fetal development occurs
vagina: the muscular tube that leads from the uterus to the external environment
vulva: the external female genital organs
zygote (fertilized egg): a single cell produced by the fusion of the egg and sperm
1.11. Lesson 3
Module 3—The Male and Female Reproductive Systems
Lesson 3—Sperm and Egg Development
 Get Focused
Get Focused
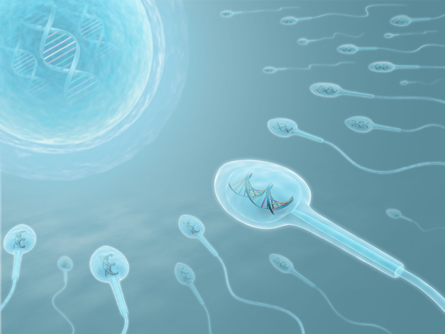
© Sebastian Kaulitzki/123RF Limited
In order for reproduction and perpetuation of the species to occur, functional gametes must be formed. To form functional gametes, supporting structures must help develop and protect the sperm and egg cells. For most couples, these structures function as they should. However, for some couples these supporting structures do not function well or at all, and problems with fertility can occur. Ultimately, infertility is the result of an abnormality in either the sperm or the egg or the body’s ability to support conception to birth.
José and Maria are the second couple in “A Fertility Case Study.” José had not been aware of any reproductive problems in his body. However, when he and Maria decided to have a baby and did not conceive, they underwent various tests to determine why they were not conceiving. One of the first fertility tests performed on a man is a sperm analysis. José’s sperm analysis showed a low sperm count.
A sperm analysis determines certain characteristics of semen and the sperm contained within the semen. An abundance of abnormalities with the sperm can result in a reduced fertility rate. Sperm must develop correctly in order to be able to successfully complete their function of fertilizing an egg cell. To gain a better appreciation of what a sperm analysis examines and how its findings indicate fertility issues, it is important to understand how gametes, both sperm and egg cells, are developed.
In Lessons 1 and 2 you learned that sperm, the functional unit of the male reproductive system, are produced and matured in the testes and that the ovum, the functional unit of the female reproductive system, is produced and matured in the ovaries. In Lesson 3 you will further your understanding of gamete development—first the sperm and then the ovum. You will investigate the following focusing questions:
-
How do sperm and egg cells develop into functional gametes?
-
What supporting structures help in the development of a fully functional gamete?
 Module 3: Lesson 3 Assignment
Module 3: Lesson 3 Assignment
Download a copy of the Module 3: Lesson 3 Assignment to your computer now. You will receive further instructions about how to complete this assignment later in the lesson.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
During this lesson you will continue the Unit B Assessment project, “A Fertility Case Study.” In addition to your lesson work, store any notes about the infertile couples you learn about in your course folder for your teacher’s feedback.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.12. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
© Jan Vancura/123RF Limited
This lesson is divided into two parts: the study of spermatogenesis and of oogenesis.
spermatogenesis: the process of spermatogonia dividing and differentiating to form mature male gametes (sperm)
oogenesis: the process of oogonia dividing and differentiating to form female gametes (eggs)
Spermatogenesis
While women are born with all the eggs they will ever have during their lifetime, men produce sperm on a continuous basis from the onset of puberty onward. Therefore, a man’s sperm development can be affected by what he does daily. Choices a man makes regarding smoking, stress management, nutrition, exercise, and drug and alcohol use contribute to the production and quality of his sperm. Regardless of the choices he makes, the quality of a man’s sperm begins to slowly decline at approximately age 25.
Gametogenesis is the formation of sex cells, or gametes, during meiosis. Human male and female gamete formation follows the same general meiotic process; however, there are significant differences, such as the number of gametes produced and how the cytoplasm is divided. Spermatogenesis is the term used to describe the process unique to sperm gamete production. Mature male gametes, commonly called sperm, are scientifically referred to as spermatozoa. During the early stages of development, germ cells and immature gametes are supported, nurtured, and protected by specialized supporting somatic cells, the Sertoli cell and interstitial cells.
Sertoli cells are found in the testes, within the seminiferous tubules, and are sometimes referred to as nurse cells. They nurture the developing sperm cells by providing secretory and structural support. By producing the hormone inhibin, Sertoli cells perform the secretory function. Inhibin targets the anterior pituitary and hypothalamus to inhibit the production of follicle stimulating hormone (FSH). The Sertoli cells also give structural support by acting as a barrier to protect the sperm during their development. The body considers sperm cells to be foreign to the body. If not protected by the Sertoli cells, the body’s immune system would destroy them.
gametogenesis: the process of creating gametes from somatic germ cells; includes meiosis
spermatozoa: mature sperm stored in the epididymis
somatic cell: a normal diploid body cell; a cell not involved in fertilization
interstitial cells: tightly packed testosterone-secreting cells that surround the seminiferous tubules in the testes
inhibin: a hormone produced by Sertoli cells during spermatogenesis that inhibits production of FSH, preventing excessive sperm production
Interstitial cells are found in the testes but are not found in the seminiferous tubules. While they are only indirectly linked to sperm production, they do secrete testosterone, which targets the entire male body and stimulates the development of the male reproductive system, the secondary male sex characteristics, and spermatogenesis.
 Read
Read
Reread section “The Testes” on pages 479 and 480 of the textbook. Focus on information about the supporting structures of the gametes.
To gain further understanding, do an Internet search using the search terms “Sertoli cells” and “interstitial cells.”
© Kiyoshi Takahase Segundo/123RF Limited
 Watch and Listen
Watch and Listen
Watch the following segments of “The Human Male Reproductive System: Perpetuating the Species” to further your understanding of how the structural support tissue helps develop the male gametes. Take notes as you watch, and save them in your course folder.
- “Semen and Ejaculation”
- “Spermatogenesis”
- “Bio Bit: Semen Components”
You may be required to enter a username and password to access the video. Contact your teacher for this information.
Oogenesis
In females, the germ cells or gametes are the egg cells. The process of developing mature egg cells is called oogenesis. Follicles are the structural supporting cells that surround and develop the egg.
oogonia: diploid cells in the ovary that will undergo meiosis
oocytes: cells that are undergoing meiosis in the ovary
primary oocytes: cells in the first meiotic division of oogenesis
Egg cells begin as oogonia and then develop into primary oocytes. About 700 primary oocytes are formed in the ovaries during fetal development. The primary oocytes stay dormant in the female body until the beginning of puberty. At the onset of puberty, some of the primary oocytes will further develop into functioning egg cells, generally at a rate of about one per month. While in the ovary, each primary oocyte is surrounded by follicles. Together the primary oocyte and the follicle cells surrounding it are referred to as the primary follicle.
Like Sertoli cells, the follicles perform a secretory and structural support function for the developing gamete. The follicles give secretory support by releasing estrogen and some progesterone. The follicles give structural support by fully surrounding the egg, thereby helping to nourish and protect the primary oocyte. When chemically stimulated to do so, the primary follicle helps develop the primary oocyte into a secondary oocyte and then into a fully functioning mature egg. Ovulation takes place when the fully matured egg is expelled from the ovary.
The support of the follicles and Sertoli cells helps ensure properly formed gametes, which can then combine during fertilization to form an embryo, thus continuing the species.
 Read
Read
Reread the section “The Ovaries” on page 482 of the textbook to review the process of oogenesis. This section of the textbook does not present much information about the role of the follicles. To gain further information, do an Internet search using the search term “follicles” or “follicle cell.”
 Watch and Listen
Watch and Listen
Watch the segment called “Oogenesis” in the video “The Human Female Reproductive System: A Creation of Exquisite Synchrony” to further your understanding of oogenesis and the role of the follicles. Take notes as you watch this video and save them in your course folder.
1.13. Page 3
Module 3—The Male and Female Reproductive Systems
 Module 3: Lesson 3 Assignment
Module 3: Lesson 3 Assignment
Retrieve the copy of the Module 3: Lesson 3 Assignment that you saved to your computer earlier in this lesson.
Complete the three drawings and three questions in the Lesson 3 Assignment when instructed to do so as you complete the following lab. When complete, save your assignment in your course folder. You will receive instructions later in this lesson about when to submit your assignment to your teacher.
 Lab—Examining Gonads and Gametes
Lab—Examining Gonads and Gametes
© Spectral-Design/shutterstock
Although the testes and ovaries are quite different structures, they serve the same two basic functions:
-
development of gametes
-
secretion of sex hormones
In this investigation you will compare ovarian and testicular tissue using microscopy (the scientific term for viewing objects with a microscope). From the images provided, you will identify the supporting structures that help develop the egg and sperm cells.
This lab is similar to the one on page 483 of the textbook. However, because you may not have a microscope, the microscope images will be provided to you. The procedure has been rewritten to guide you through the lab using the microscopic images.
Problem (Purpose)
How do the structures of testicular and ovarian tissues relate to their biological functions?
Materials
-
blank paper
-
pencil
-
microscopy images of testis: 100X, 200X, 400X (provided below)
-
microscopy images of cat follicle: 100X, 200X, 400X (provided below)
Procedure
Part 1—Testicular Tissue
Step 1: View the microscopy and other model images of the testes below. Where it is provided, pay attention to the magnification power given.
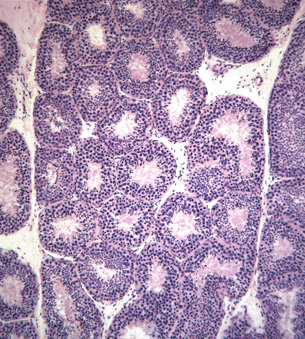
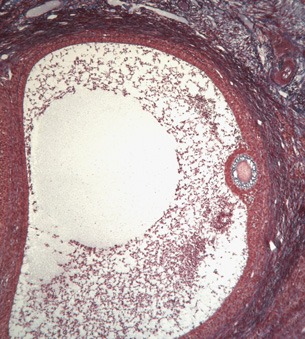
Microscope image of a cross-section of a seminiferous tubule at 100X magnification
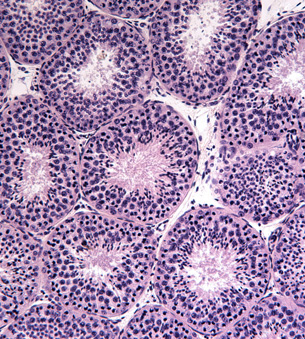
Microscope image of a cross-section of a seminiferous tubule at 200X magnification

Microscope image of a cross-section of a seminiferous tubule at 400X magnification
Step 2: Read “Appendix D: Review of Biological Drawings” on page 759 of the textbook. Follow the instructions given when making the biological drawings requested in this lab.
Step 3: Search the Internet for images of the internal structure of the testes. You could start your search using the phrase "seminiferous tubules male reproductive system anatomy." Use results from medical schools to study the internal structures.
Step 4: Examine the microscopy images provided above. Look for several circular structures. These are the seminiferous tubules. Try to identify the following cells in the images: lumen, seminiferous tubule wall, spermatogonial cells, spermatocytes, spermatids and spermatozoa or mature sperm cells, Sertoli cells, and interstitial cells.
- Draw a diagram of the specimen as it appears under the highest power magnification. Label the following cells in your drawing: lumen, seminiferous tubule wall, spermatogonial cells, spermatocytes, spermatids and spermatozoa, Sertoli cells, and interstitial cells. If possible, paste your image into the space provided for question 1 in your Lesson 3 Assignment document; otherwise, submit your drawing to your teacher when instructed to do so later in this lesson.
Part 2—Ovarian Tissue
Step 5: View the microscopy and other model images of the ovaries below. Where it is provided, pay attention to the magnification power given.
Step 6: Search the Internet for images of the internal structure of the ovary. You could start your search using the phrase "human female reproductive system histology." Use results from medical schools to study the internal structures.
Step 7: Examine the microscopy images provided below. Look for larger circular structures; these are developing egg cells. Try to identify the following structures in the images: primary follicle, primary oocyte, mature follicle, mature ovum, ovarian tissue, and corpus luteum.
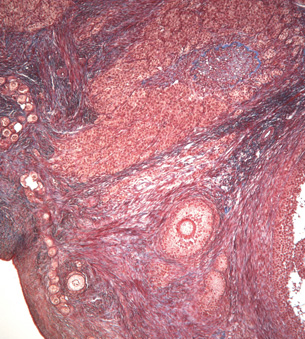
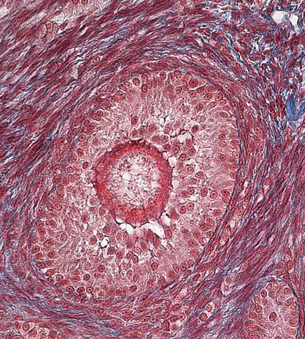
Microscope images of a cross-section of a cat ovary showing a primary follicle at 100X magnification
Microscope image of a cross-section of a cat ovary showing a view of a mature follicle at a 100X magnification
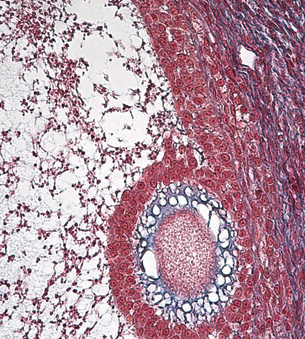
Microscope image of a cross-section of a cat ovary showing a view of a mature follicle at a 400X magnification
-
Draw a diagram of the specimen image, Cat, Primary Follicle, 100X. Label the following structures in your drawing: primary follicle, primary oocyte, ovarian tissue, and corpus luteum. If possible, paste your image into the space provided for question 2 in your Lesson 3 Assignment document. Otherwise, submit your drawing to your teacher when instructed to do so later in this lesson.
-
Draw a diagram of the specimen image, Cat, Mature Follicle, 100X. Label the mature oocytes and follicle cell structures in your drawing. If possible, paste your image into the space provided for question 3 in your Lesson 3 Assignment document. Otherwise, submit your drawing to your teacher when instructed to do so later in this lesson.
Observations
After examining the microscopy slides of testicular and ovarian tissues, you should have completed three diagrams with appropriate labels and titles. You should now be able to identify the functional gametes as well as their supporting structures.
Questions
Answer the questions 4 through 6 in the Lesson 3 Assignment document using knowledge from examining the gonad tissue sample images.
Conclusions
In this lab you identified the location and function of the gonads, gametes, and their supporting structures. Reproduction and, therefore, continuation of the species would be impossible if not for proper functioning of the supporting cells that develop the gametes.
Real-World Applications (Going Beyond)
In this lab you have seen gonad tissue and identified some of the structures within these organs. Things are never quite as simple as they seem; there are other structures that have not been mentioned in this lab or in your textbook. See if you can research and add the following structures to your diagrams: testicular basement membrane, blood-testis barrier, blood vessels, early spermatid, late spermatid, corpus albicans, early and mature corpus luteum, primordial follicles, follicular cavity, follicular fluid, zona pellucid, and corona radiate.
 Self-Check
Self-Check
Complete “Section 14.1 Review” questions 1 to 4 and 6 to 8 on page 485 of the textbook to see how well you understand the development of the egg and sperm cells.
 Self-Check Answers
Self-Check Answers
“Section 14.1 Review” Answers
- The two main purposes of the gonads are to produce gametes and to secrete sex hormones.
- a. fimbriae: found in the female reproductive system; it is responsible for helping to move the ovum (released during ovulation) into the oviduct. It sweeps over the ovary and moves the ovum into the cilia-lined oviduct.
b. ductus deferens: found in the male reproductive system; it is a storage duct responsible for storing and eventual transport of sperm to the urethra during ejaculation.
c. endometrium: found in the female reproductive system; it is the uterine lining that will support an implanted embryo.
d. epididymis: found in the male reproductive system, it stores the sperm during maturation and as they become motile. Once matured, the sperm move to the ductus deferens
- Sperm move out of the epididymis into the ductus deferens, where they are mixed with various fluids to make semen. The seminal vesicles provide a mucus-like fluid containing fructose for energy; the prostate gland and Cowper's gland provide alkaline and mucus-like fluids that can neutralize the acids in the female reproductive tract. The combination of sperm and the fluids make up semen.
- The ovum is moved from the ovary into the oviduct with the aid of the fimbriae, which are thread-like projections. As the egg moves down the oviduct it is aided by the beating of the cilia. This creates a current that moves the ovum towards the uterus.
- a. an oocyte
b. follicle
c. ovarian tissue
- The sperm is composed of three parts: a head, a mid-section, and a tail. The tail provides the motility required to move the sperm through the female reproductive tract; the tail is powered by a middle section that has mitochondria that can use the fructose provided by the seminal vesicles to make energy. The head section carries both the chromosomal material and the acrosome (a cap-like structure that contains the enzymes needed to penetrate the jelly-like layer surrounding the egg). The much larger, round ovum is covered by a specialized layer that only allows sperm with acrosome enzymes to penetrate. The egg has no structures to support motility, making it a more accessible target for the sperm, and its larger size makes it easier for the tiny sperm to attempt to fertilize it. The egg also contains cytoplasm and organelles to support the zygote as it makes its way into the uterus to implant itself in the endometrium.
- By wearing looser pants, his scrotum will be further away from his body and at a temperature more conducive to the production of viable sperm—35°C as opposed to the usual 37°C. High temperatures can cause deformed sperm to mature, as well as decrease the number of sperm produced.
1.14. Page 4
Module 3—The Male and Female Reproductive Systems
 Reflect and Connect
Reflect and Connect
Update: A Fertility Case Study
Think back to José and the semen analysis test he underwent. From your new knowledge of how supporting structures help gametes develop, you can better understand how a semen analysis can contribute to diagnosing an infertility problem.
A semen sample must be analyzed within two hours of being collected. Lab technicians analyze the sample for the following traits:
- volume: Low volume might suggest an anatomical or functional defect.
- motility: The quality of spermatozoa movement needs to be forward and progressive, and 40% to 60% of the spermatozoa need to be motile.
- count: A count below 20 million/mL could indicate sterility.
- pH: An increase in the sperm's pH above the normal slightly alkaline state could indicate an inflammation of the prostate.
- fructose: Absence of this sugar may indicate a possible obstruction of the ejaculatory ducts or seminal vesicles.
- morphology (size and shape): Only 35% or less of the sperm should have some type of abnormal structure, as seen in the following image.

oligospermia (oligozoospermia): a condition in which there are less than 20 million spermatozoa per millilitre of semen
José’s sperm analysis showed a low sperm count. The medical term for this is oligospermia. If you were José’s fertility physician, you might have considered prescribing a drug called clomiphene, which is sold under the name Clomid.
 Reflect on the Big Picture
Reflect on the Big Picture
Understanding how the structures that support the egg and sperm develop properly functioning gametes is essential to understanding the functions of the male and female reproductive systems.
Continue to make notes about the couples’ fertility problems, specifically those of José. Do an Internet search to learn more about oligospermia and the drug Clomid. Save your notes, including conclusions or assumptions, in your course folder. Remember that information and questions about the couples’ fertility issues will be referred to throughout Unit B and will be part of the Unit B Assessment.
 Going Beyond
Going Beyond
corpus luteum: the structure that develops from a matured follicle that has released its egg
The corpus luteum produces progesterone and some estrogen. If pregnancy does not occur, the corpus luteum degenerates.
You have been introduced to several disorders in the first three lessons of Module 3. Can you find disorders that are specifically related to the supporting structures like the Sertoli cells, interstitial cells, primary or secondary follicles, and corpus luteum?
 Module 3: Lesson 3 Assignment
Module 3: Lesson 3 Assignment
Submit your completed Module 3: Lesson 3 Assignment to your teacher for assessment.
1.15. Page 5
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In Lesson 3 you investigated the following focusing questions:
-
How do sperm and egg cells develop into functional gametes?
-
What supporting structures help in the development of a fully functional gamete?
Human reproductive systems are uniquely designed to develop properly functioning gametes, thereby ensuring continuation of the human species. In the male reproductive system, the male gonads (the testes) produce the functional gametes (the sperm) in the seminiferous tubules. The Sertoli cells give both structural and secretory support to the developing sperm. Structural support is provided by protecting the developing sperm from the body’s immune system, and secretory support is provided by secreting the hormone inhibin. The interstitial cells, also found in the seminiferous tubules, indirectly support sperm production by secreting the hormone testosterone. Testosterone then stimulates the process of spermatogenesis to develop the sperm.
The female gamete, the egg, is produced in the ovary and provided with structural and secretory support. Follicles provide structural support by surrounding the primary oocyte, helping to nourish, protect, and develop the egg cell. Follicles also offer secretory support by releasing estrogen and some progesterone. These hormones then help to develop the primary oocyte into a mature egg that is ready for ovulation.
Continuation of the species is ensured when these two properly formed gametes are joined through fertilization.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
corpus luteum: the structure that develops from a matured follicle that has released its egg
The corpus luteum produces progesterone and some estrogen. If pregnancy does not occur, the corpus luteum degenerates.
gametogenesis: the process of creating gametes from somatic cells; includes meiosis
inhibin: a hormone produced by Sertoli cells during spermatogenesis that inhibits GnRH, preventing excessive sperm production
interstitial cells: tightly packed testosterone-secreting cells that surround the seminiferous tubules in the testes
oligospermia (oligozoospermia): a condition in which there are less than 20 million spermatozoa per millilitre of semen
oocytes: cells that are undergoing meiosis in the ovary
oogenesis: the process of egg production in females
oogonia: diploid cells in the ovary that will undergo meiosis
primary oocytes: cells in the first meiotic division of oogenesis
somatic cell: a normal diploid body cell; a cell not involved in fertilization
spermatogenesis: the process of sperm production in males
spermatozoa: mature sperm stored in the epididymis
1.16. Lesson 4
Module 3—The Male and Female Reproductive Systems
Lesson 4—Chromosome and Hormone Influence
 Get Focused
Get Focused

© Willee Cole/BigStockPhoto
The first couple in “A Fertility Case Study,” Jane and John, decided not to have children until they were in their early thirties. Their first pregnancy produced gender-different twins, also called fraternal or dizygotic (di, meaning “two;” zygotic, meaning “zygote”) twins. In fraternal twins, each embryo has a unique makeup because it comes from a separate egg fertilized by a separate sperm. Gender is dependent on the chromosomal makeup of the embryos, and fraternal twins are often different sexes.
To maintain the variation and continuation of a mammalian species, such as the human species, two separate genders are required. In a species with two genders, there are two different sex chromosomes at play—the X and Y chromosomes. These are referred to as sex chromosomes because they determine the gender, or sex, of the offspring. To be a male, an organism must have one X chromosome and one Y chromosome (XY). To be a female, an organism must have two X chromosomes (XX). Further information about the structure and function of chromosomes will be provided in Unit C.
The gender of a child is determined at conception by the genetic material carried in the sperm. While all eggs carry the X chromosome, a sperm can carry either an X or a Y chromosome. Although it was once believed that female development would just occur unless “maleness” was stimulated by the presence of the Y chromosome, researchers now think the process of becoming female is much more intricate.
While the genders of Jane and John’s twins were determined at conception, they remained identical in gender until about the sixth or seventh week of their embryonic development. At this point, the sex-determining region Y (SRY) carrying the testis determining factor (TDF) gene, found on the Y chromosome of their male fetus, began the process that leads to the sexual development of a male individual. The TDF gene started the production of the male sex hormones, collectively called androgens, which began the development of the male sex organs. The lack of the Y chromosome with the TDF gene and the resulting male sex hormones allowed the other fetus to develop as female.
To develop the male twin, the TDF gene caused differentiation of the supporting cells into Sertoli cells and interstitial cells. The interstitial cells begin to form the hormone testosterone by about the eighth week of gestation. From the eighth to the twelfth week of gestation, the testosterone caused the gender identical structures to differentiate into male structures—such as testes, penis, and scrotum. Although the way in which an embryo becomes female is not fully understood, it does appear that without the presence of testosterone and other hormones to suppress the development of female sex characteristics, other hormones then cause female reproductive structures to develop.
Although the ways in which embryos develop as male or female differ, both are controlled by genes and hormones. For the twins, their genders were determined at conception, and sex characteristics developed as they underwent fetal growth. They will not display all of their gender-specific characteristics until they reach puberty. You will learn more about puberty later in Module 3.
gender: the sex of an organism
fraternal (dizygotic) twins: twins produced when two different eggs are fertilized by two different sperm; not identical and may be of different genders
sex chromosomes: the twenty-third pair of chromosomes that determines gender
XX is female, XY is male.
X chromosome: the larger sex chromosome with many more genes than Y
Y chromosome: a small sex chromosome that contains the TDF gene; determines maleness of fetus
testis determining factor (TDF): a protein produced by a gene on the Y chromosome, which results in male primary sex characteristics
androgens: male group of steroid hormones; includes testosterone
testosterone: male sex hormone secreted by interstitial cells of the testes; results in male primary and secondary sex characteristics
gestation: the period of pregnancy
sex characteristics: structures and characteristics that differentiate one gender from the other
puberty: the period when reproductive abilities begin
In Lesson 4 you will learn the roles of the X and Y chromosomes and the hormones they produce to better understand gender differentiation and general hormone changes during puberty. You will investigate the following focusing questions:
- How is gender determined at conception?
- How do the X and Y chromosomes and hormonal influences form gonads and reproductive organs in the female and male embryo and fetus?
 Module 3: Lesson 4 Assignment
Module 3: Lesson 4 Assignment
There is no assignment for this lesson. As the influence of the male and female chromosomes and their hormones is not complete in forming male and female characteristics until after puberty, the assessment for the material presented in this lesson will be included in a later lesson assignment.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
While you are completing this lesson, there will be many opportunities for you to acquire, understand, and practise the concepts that are presented to you. As you complete these activities, as well as your summary notes, you will file everything in your course folder to reference when you are preparing for exams.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.17. Page 2
Module 3—The Male and Female Reproductive Systems

© Kandi Traxel/BigStockPhoto
 Explore
Explore
 Read
Read
Read “Sex Hormones and the Male Reproductive System” on pages 492 and 493 of the textbook and “Sex Hormones and the Female Reproductive System” on page 495 to begin your understanding of gender development in the fetus. Further hormonal regulation of sexual development will be dealt with later in Module 3. You may summarize your reading in a comparative chart to be saved in your course folder.
 Try This
Try This
Work through the “Gender Testing of Female Athletes” activity.
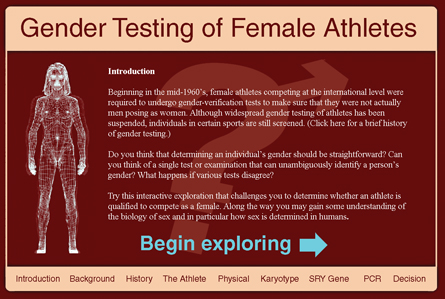
© 2008 Howard Hughes Medical Institute
1.18. Page 3
Module 3—The Male and Female Reproductive Systems
 Reflect and Connect
Reflect and Connect
From the time a pregnancy is confirmed, everybody wonders if the developing baby will be a boy or a girl. Normal embryonic sex determination is a complex process requiring that numerous events take place in the correct order. If all events proceed successfully, a “gender-normal” boy or girl will be born. You know that if two X chromosomes combine at conception, the zygote will develop into a female, and if one chromosome is X and the other is Y, then the zygote will develop into a male. Reflect on how that unicellular zygote develops into a multicellular organism with special sex characteristics. Later in the unit you will examine the factors that contribute to the translation of XX or XY into a sexual individual. Your understanding of the development of Jane and John’s twins into one female and one male child should be falling into place.
 Discuss
Discuss
Choose one, some, or all of the following questions to discuss with your peers and teacher.
D 1. What is the advantage of having more than one gender in a species?
D 2. Historically, women have been held responsible for not producing male children. How has science helped to change this view? Are there places where the historical view is still held?
D 3. Should gender be tested for at birth? Why or why not?
D 4. Are there ways to predict whether a pregnancy will result in a boy or girl before the birth?
D 5. How many sex chromosomes does a platypus have?
After reviewing the responses of other students to the questions, has your view or understanding changed? Is so, how? Record a reflection in your course folder.
 Reflect on the Big Picture
Reflect on the Big Picture
For Jane and John, having different gendered twins was a great way to start their family. However, during the twins’ development into one male and one female embryo, an abnormality developed in the female fetus. She was born with only one X chromosome, a condition called Turner syndrome. The explanation for and results of this missing chromosome will be discussed in Unit C.
Keep track of what is happening with Jane and John by recording the information you learned about their experience in your course folder.
 Going Beyond
Going Beyond
You may have noticed that there are often exceptions to the rule in biological studies. This is the case with respect to the X and Y chromosomes that determine gender. It is possible during gamete formation that the TDF gene can be transferred incorrectly or can be missing altogether. Conduct research to find out how individuals can be male with a genotype of XX and female with a genotype of XY.
 Module 3: Lesson 4 Assignment
Module 3: Lesson 4 Assignment
There is no assignment for this lesson.
1.19. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In Lesson 4 you investigated the following focusing questions:
-
How is gender determined at conception?
-
How do the X and Y chromosomes and hormonal influences form gonads and reproductive organs in the female and male embryo and fetus?
Sexual reproduction is necessary to provide variation in a species. The formation of male and female genders in embryos is a complex process that is influenced by chromosome structure and the secretion of sexual hormones. Since all eggs carry the X chromosome, and the sperm carries either an X or a Y chromosome, the male parent determines gender. Typically, for an organism to be male, it must carry the XY sex chromosomes; for an organism to become female, it must carry the XX sex chromosomes. Once the chromosomal structure of the individual is determined, various hormones continue the sexual development of the embryo.
For a male embryo to develop the SRY region with the TDF gene, a chain of events begins that leads to the production of testosterone and the eventual outcome of a male fetus. Although the process is not fully understood, the chain of events that leads to the development of a female embryo occurs due to lack of testosterone and other male hormones. Ovaries and the hormones they produce lead to the development of a female fetus.
Gender determination begins at conception but continues through to puberty, when the final stages of sex determination are completed. Different genders within a species ensure variation and, ultimately, continuation of a species.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
androgens: male group of steroid hormones; includes testosterone
fraternal (dizygotic) twins: twins produced when two different eggs are fertilized by two different sperm; not identical and may be of different genders
gender: the sex of an organism
gestation: the period of pregnancy
puberty: the period when reproductive abilities begin
sex characteristics: structures and characteristics that differentiate one gender from the other
sex chromosomes: the twenty-third pair of chromosomes that determines gender
XX is female, XY is male.
testis determining factor (TDF): a protein produced by a gene on the Y chromosome, which results in male primary sex characteristics
testosterone: male sex hormone secreted by interstitial cells of the testes; results in male primary and secondary sex characteristics
X chromosome: the larger sex chromosome with many more genes than Y
Y chromosome: a small sex chromosome that contains the TDF gene; determines maleness of fetus
1.20. Lesson 5
Module 3—The Male and Female Reproductive Systems
Lesson 5—Sexually Transmitted Infections and Fertility
 Get Focused
Get Focused

The lessons in Module 3 so far have emphasized that continuation of a species is dependent on reproduction. Sexual reproduction offers the highest advantage for continuation of a species because it ensures diversity.
In order for sexual reproduction to occur, there has to be an exchange of body fluids. Whenever there is an exchange of body fluids, there is the chance of acquiring or spreading an infection. Infections that are transmitted by sexual contact are referred to as sexually transmitted infections or STIs. Names like sexually transmitted diseases (STDs) and venereal disease (VD) are also used to identify this group of disorders; however, the health care community prefers the term infection over the term disease because a person can be infected without showing any signs or symptoms. Even a symptom-free person can pass his or her infection on through sexual contact. Sexually transmitted infections can also be transmitted from mother to child during childbirth and breastfeeding. Sexually transmitted infections pose a risk not only to the individual, but also to the species as a whole. Just think of the effect of the HIV/AIDS epidemic, especially in countries such as Africa.
body fluids: primarily semen, vaginal fluid, saliva, and blood
STI: sexually transmitted infection due to bacteria, fungus, or viruses; may not cause symptoms, but is still contagious
STD: a sexually transmitted disease caused by bacteria, fungus, or virus
The transmission of the disease does cause symptoms.
venereal: referencing the genitals or external sex organs
The Public Health Agency of Canada warns that some of the highest rates and increases in STIs in Canada are in young people ages 15 to 24.
You have a tremendous amount of control and choice over your personal sexual conduct and contact. Having choice also means having great responsibility. As you move through puberty and discover your sexual nature, remember that bad decisions can sometimes result in severe, lifelong consequences. Although not all STIs are lifelong or life-threatening, some are. It is crucial that you understand your own reproductive health, the structures and functions of the human reproductive system, and the consequences of acquiring an STI in order for you to make good life choices.
cancer: uncontrolled cell division resulting in tumours that may be life-threatening
endometriosis: excessive buildup of the endometrial lining of the uterus
ovarian cysts: fluid-filled swellings on the ovary
impotence: inability to sustain an erection
pelvic inflammatory disease (PID): an infection in the uterus and surrounding tissues; may result in scarring and/or infertility
toxic shock syndrome: a rare, rapidly developing, and potentially fatal bacterial infection of the vagina; associated with extended tampon use
Sexually transmitted infections are not the only threat to the homeostatic reproductive balance affecting fertility. Disorders such as cancer, endometriosis, ovarian cysts, impotence, pelvic inflammatory disease (PID), and toxic shock syndrome can also affect fertility.
Cancer is a term used to describe a large number of diseases where rapid, uncontrolled cell division occurs. You will learn more about this uncontrolled cell division in Unit C. Cancer can affect fertility in two ways: the disease itself may target and damage specific reproductive structures, and the treatment of the disease in other parts of the body can damage reproductive structures and functions. The most common cancers to directly target reproductive structures and affect fertility are prostate and testicular cancers in males; and cervical, ovarian, and uterine cancers in females. Breast cancer, a common cancer affecting both men and women, does not directly affect fertility. Common cancer treatments that affect fertility use specific technologies that you will study in this course. These include certain chemotherapies, bone marrow or stem cell transplants, radiation treatment, and specific types of surgery. Even the future fertility of a child undergoing cancer treatment may be a concern. Cancer does not always mean an end to fertility—there are many, many cancer survivors who go on to have normal reproductive health, including having children.
chemotherapies: drug therapies designed to poison and kill cancer cells but spare normal cells
bone marrow transplant: a procedure in which bone marrow from a donor is used to “seed” new bone marrow in blood and bone marrow cancer patients
stem cell transplant: transplant of a donor's stem cells from sources such as bone marrow or umbilical cord blood; used to treat cancers of the blood and bone marrow
radiation treatment: ionizing radiation directed at tumours to destroy cancer cells
surgery: performing an operation on a patient using instruments; in cancer, the removal of tumours and affected tissues
To their surprise, many couples experience fertility problems due to STIs or cancers. Olga and Karl, the third couple in “A Fertility Case Study,” were each married to other people before marrying each other. Karl has two children from his previous marriage. Although Olga did not bring any children into her marriage to Karl, she had attempted, without success, to have children in her first marriage. Olga and Karl have been trying to have a child together for two years with no success. The typical first set of fertility tests and blood tests have proven that there are no problems with either of their hormone levels.
antibodies: blood proteins that bind to and destroy infectious antigens such as bacteria and viruses
As their fertility doctor, you want to start the next set of tests on Olga. You want her to have one more blood test—a test that will detect antibodies related to some common STIs. These antibodies can cause blockage of the Fallopian tubes. At first Olga is upset to hear that you suspect she may currently have or have had an STI. She knows very little about them. As her physician, it is your obligation to explain what the blood test will look for and how STIs can affect fertility.
You can uncover a wealth of information about sexually transmitted infections using the search terms “sexually transmitted infections” and “sexually transmitted diseases” in an Internet search.
In Lesson 5 you will explore how disorders, specifically sexually transmitted infections, compromise structural fertility. You will investigate the following focusing question:
-
How do diseases and sexually transmitted infections compromise structural fertility?
 Module 3: Lesson 5 Assignment
Module 3: Lesson 5 Assignment
Download a copy of the Module 3: Lesson 5 Assignment to your computer now. You will receive further instructions on how to complete this assignment later in the lesson. Because the Module 3 Assessment addresses sexually transmitted infections in general, the assignment for this lesson will address reproductive cancers.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
During this lesson you will continue the Unit B Assessment project, “A Fertility Case Study.” In addition to your lesson work, store any notes you make about the infertile couples in your course folder for your teacher’s feedback.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.21. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
You may choose to do either the Read or the Watch and Listen activity. As you review the material about STIs, pay particular attention to the effects they can have on the reproductive structures and their functions. The video provides a general overview while the reading is more detailed. As you choose to complete the reading or watch the video, begin the Try This activity. The completed table will become your notes about STIs.
 Try This
Try This
Complete the table about sexually transmitted infections. The first row has been completed as an example.
 Read
Read
Sexually transmitted infections have plagued humans for thousands of years. They can affect anyone at any time regardless of gender, age, race, wealth, religion, or culture. In order to make informed choices regarding your reproductive health, you must be aware of the main causes and effects for the most common STIs.
This lesson will only address seven of the most common, serious, and rapidly spreading STIs. There are many other STIs, cancers, and other reproductive disorders that can affect fertility.
Read “Effect of STIs on the Reproductive Systems” on pages 486 to 490 in the textbook.
 Watch and Listen
Watch and Listen
Watch the video “Reproductive Technologies and Sexually Transmitted Diseases: Eggs, Embryos, and Ethics” to learn more about the causes, signs and symptoms, transmission, consequences, and treatments of some of the more common sexually transmitted infections.
 Self-Check
Self-Check
SC 1. Examine the following graphs detailing infection rates of certain STIs by age group in Alberta. For each graph, write an interpretation of the data presented by examining the age group and rate of infection.
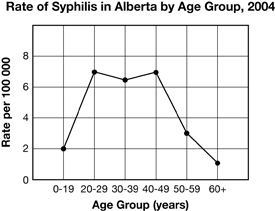
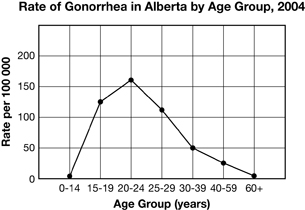
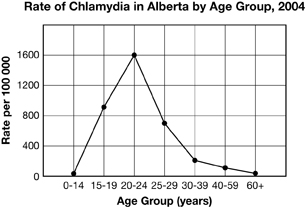
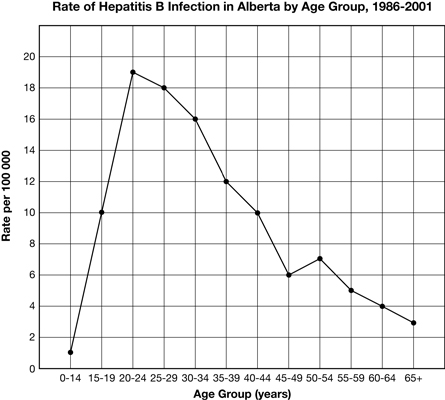
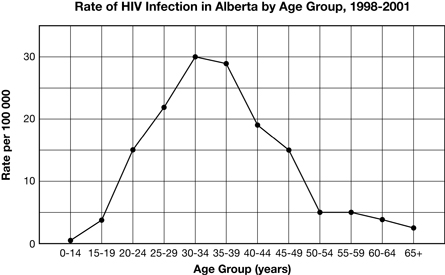
 Self-Check Answers
Self-Check Answers
SC 1.
Rate of Syphilis Graph: Syphilis infection predominantly affects individuals who are 20 to 49 years of age. However, the incidence of syphilis is low compared to other sexually transmitted infections.
Rate of Gonorrhea Graph: Gonorrhea infection is highest among the 20 to 24 age group, but the 15 to 19 and 25 to 29 age groups also have a relatively high rate of infection.
Rate of Chlamydia Graph: The rate of chlamydia infection is very high among the 20 to 24 age group. The rate of infection among the 15 to 19 age group and the 25 to 29 age group is nearly half that of the 20 to 24 age group, but is still very high compared with other sexually transmitted infections.
Rate of Hepatitis B Graph: The rate of hepatitis B infection rises dramatically from the 0 to 14 age group and the 20 to 24 age group. It decreases gradually from age 25 to 65+, with a slight increase in the 50 to 54 age group.
Rate of HIV Infection Graph: HIV infection is highest among the 30 to 39 age group. It is less common than chlamydia and gonorrhea among this age group. Individuals aged 0 to 19 and 50 to 65+ have a relatively low rate of HIV infection.
 Discuss
Discuss
Although STIs can be a difficult topic to discuss, it is important to make sure you have a good understanding of what they are and how they are transmitted. Use the discussion area of your class to discuss one, some, or all of the following questions.
D 1. Why is it so difficult for teens and young adults to believe they can acquire an STI?
D 2. How would you get the message of the seriousness of STIs across to young people?
D 3. If a person tests positive for an STI, should health agencies have the right and responsibility to inform the individual’s sexual partners? Why or why not?
D 4. Can the use of a condom prevent all STIs?
 Self-Check
Self-Check
SC 2. See how well you understand STIs by completing “Section 14.2” questions 1 to 6 on page 491 of the textbook.
 Self-Check Answers
Self-Check Answers
“Section 14.2 Review” Answers
1. Examples of Viral and Bacterial STIs
| Viral STIs | Bacterial STIs |
| HIV/AIDS | chlamydia |
| hepatitis (A, B, and C) | gonorrhea |
| genital herpes | syphilis |
| HPV |
2. PID (pelvic inflammatory disease) is a disease that occurs in women; it is caused by undetected chlamydia that has spread to the cervix and oviducts. PID is painful and can lead to the buildup of scar tissue in the oviducts and open sores on the cervix. This may lead to infertility (oviduct damage) and/or an increased risk of acquiring HIV. Chlamydia and PID also pose risks to babies who come into contact with the disease during birth, including potential respiratory infections and eye infections. PID can also arise if gonorrhea goes untreated.
3. A woman who is infected with an STI can present numerous risks to her baby. Diseases can be passed to the baby through the placenta (e.g., HIV, hepatitis B), during birth (e.g., HIV, genital herpes, chlamydia, gonorrhea), and through breast milk (e.g., HIV).
4. a) A person who is infected with an STI but does not present any symptoms will not visit a doctor for treatment. While they wait, the infection may become more serious, progressing to PID, infections, cancer of the cervix (women), tumors on the vulva, vagina, anus or penis, or infertility.
b) The public health risk of the asymptomatic individual infected with an STI is that they may unknowingly infect other people if they engage in unsafe sex practices or, in the case of pregnant women, pass the STI to their babies.
5. Look for the following key points: Both viral and bacterial STIs have health consequences, the severity of which increases as the infection progresses untreated, and depending on the type of infection. It is true that the viral infections cannot be cured, only managed, and there is a high likelihood that death will result with some viral infections (HIV and hepatitis) or that cancer may develop (HPV). Bacterial infections, while curable, are more likely to go undetected, increasing the possibility that they will be spread unknowingly, as well as the possibility that they won't be detected until they have progressed to the more damaging PID, which can cause scarring and infertility, or infect a baby during birth. In addition, many bacterial diseases are becoming resistant to current antibiotics. The consequences of either form of STI make it preferable to avoid both.
6. a) Points supporting the teaching of abstinence: abstinence (from oral, anal, and vaginal sex, and the sharing of needles) is the only way to guarantee the prevention of transmission of STIs. Points supporting the teaching of safe sex practices: students may argue that individuals will engage in sexual practices so it is better to be educated about safe sex practices to avoid transmission of STIs (as well as unwanted pregnancies). Students can evaluate the arguments from an individual point of view, a societal point of view, or even a government viewpoint. It is in the best interest of society and government to teach people about the effects and transmission of STIs so that healthcare does not have to deal with large volumes of transmissions.
b) Health practitioners can design education campaigns that respect the views of those advocating abstinence and safe sex practices by presenting the facts of each and allowing the recipients of the information to make their own decision. This can be done by avoiding nuanced language or judgmental, subjective conclusions.
Inquiry into Biology TRG (Whitby, ON: McGraw-Hill Ryerson, 2007), Sec 14.2 Reproduced by permission.
viral STIs: examples are HIV, HPV, and hepatitis; more problematic, possibly incurable because they cannot be treated with antibiotics
bacterial STIs: examples are gonorrhea, syphilis, and chlamydia; can be treated with antibiotics
asymptomatic infection: infection that is present but the affected person does not experience symptoms
abstinence: not having sexual intercourse
safe sex: the use of a barrier, such as a condom, during sex to prevent transmission of infection
1.22. Page 3
Module 3: Section 1—The Male and Female Reproductive Systems
 Reflect and Connect
Reflect and Connect
 Module 3: Lesson 5 Assignment
Module 3: Lesson 5 Assignment
Because the Module 3 Assessment addresses sexually transmitted infections in general, the assignment for this lesson will address reproductive cancers.
In Olga and Karl’s ongoing fertility assessments, they were asked whether their families had a history of cancer or other hereditary disorders. This kind of information is used to establish possible risk levels for some cancers. Like many of you, both Olga and Karl had an extended family member diagnosed with cancer. Olga and Karl went to their local Canadian Cancer Society office to learn more about reproductive cancers.
Retrieve the copy of the Module 3: Lesson 5 Assignment that you saved to your computer earlier in this lesson. Complete the assignment. Save your completed assignment in your course folder. You will receive instructions later in this lesson about when to submit your assignment to your teacher.
 Self-Check
Self-Check
SC 3. As Olga and Karl's fertility doctor you have decided to test Olga for an STI, but not to test Karl. What past evidence indicates that you may not have to test Karl for an STI?
 Self-Check Answers
Self-Check Answers
SC 3. Sexually transmitted infections and their effects on the body, even after treatment, can cause infertility. In Olga’s first marriage, she and her husband tried unsuccessfully to have children. Her infertility may be caused by damage from an STI. Karl has fathered two children and his fertility was not in question. He has tested negative for the presence of STIs.
 Reflect on the Big Picture
Reflect on the Big Picture
Update: A Fertility Case Study
Anyone can acquire an STI or be affected by other reproductive disorders. It is common for these to go undetected until a couple has problems conceiving or an individual experiences symptoms. As a result, an infected person can pass on his or her STI before knowing that he or she is infected. Without early treatment, the infection can also lead to further disorders, as in Olga’s case.
Olga’s STI blood test showed chlamydia antibodies, proving she had a chlamydia infection at some point in the past. Further tests showed that the infection was no longer present.
ultrasound: a medical diagnostic technique in which high-frequency sound waves are bounced off body structures to obtain an image
laparoscopy: a non-invasive surgical technique using cameras, specialized tools, and small incisions
Olga is one of the 75% of women who do not show symptoms and are unaware of their infection. Left untreated, Olga’s infection spread to her Fallopian tubes and caused pelvic inflammatory disease (PID), which was confirmed through a pelvic ultrasound and laparoscopic surgery. Pelvic inflammatory disease caused permanent damage to Olga’s Fallopian tubes by turning normal tissue into scar tissue, which blocked the tube and is the ultimate cause of her infertility.
Continue to make notes about the couples’ fertility problems, specifically those of Olga and Karl. Save your notes, including conclusions or assumptions, in your course folder. Remember that information and questions about the couples’ fertility issues will be referred to throughout Unit B and will be part of the Unit B Assessment.
 Going Beyond
Going Beyond
yeast infection: candidiasis; a common form of fungal infection of the vagina or penis; characterized by itch, redness, and discomfort
Hundreds of clinics, websites, and institutes deal exclusively with reproductive problems because of the many, many causes for imbalance in the human reproductive system. Research other reproductive disorders, such as endometriosis, ovarian cysts, impotence, yeast infections, and toxic shock syndrome. Use these terms and “human reproductive science” as Internet search terms.
 Module 3: Lesson 5 Assignment
Module 3: Lesson 5 Assignment
Submit your completed Module 3: Lesson 5 Assignment to your teacher.
1.23. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In Lesson 5 you investigated the following focusing questions:
-
How do diseases and sexually transmitted infections compromise structural fertility?
Given the many possible problems that can occur in human reproductive systems, it is amazing that healthy babies are born every day. Humans are constantly affected by structural and hormonal problems due to STIs and other disorders, sometimes without even knowing it. Yet the species continues. There are now more than six billion human beings on the planet! Our reproductive strategy is obviously working.
Young Canadians in the 15 to 25 age group have some of the highest rates of STIs in the country. Sexually transmitted infections are not only passed between sexual partners, but can also be spread from mother to child during childbirth and breastfeeding. Many STIs are lifelong infections with few to no treatment options.
While cancer itself is not directly transmitted through the sharing of body fluids, like STIs, it is a disorder that affects fertility. The rate of cancer diagnoses is on the rise. The World Health Organization (WHO) states that global cancer rates could increase by 50% to 15 million new cases by 2020. Even though these numbers are for all types of cancers, because they include reproductive cancers, it can be assumed that reproductive cancers are also on the rise. WHO further states that up to 23% of malignancies in developing countries are caused by infectious agents, including hepatitis B and C viruses and human papillomaviruses. These infectious agents can lead to the development of cervical cancer. Developed countries, like Canada, have a much higher cervical cancer detection rate than underdeveloped countries. As a result, women in developed countries are less likely to die from this disease. One tool used for early detection and treatment of cervical cancer is the PAP smear. Women are encouraged by their doctors to have a PAP smear every year.
To maintain your overall health, your chances of having your own children, and the safety of any future sexual partners, it is imperative that you understand the facts surrounding STIs and make good choices regarding your reproductive health.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
abstinence: not having sexual intercourse
antibodies: blood proteins that bind to and destroy infectious antigens such as bacteria and viruses
asymptomatic infection: infection that is present but the affected person does not experience symptoms
bacterial STIs: examples are gonorrhea, syphilis, and chlamydia; can be treated with antibiotics
body fluids: primarily semen, vaginal fluid, saliva, and blood
bone marrow transplant: a procedure in which bone marrow from a donor is used to “seed” new bone marrow in blood and bone marrow cancer patients
cancer: uncontrolled cell division resulting in tumours that may be life-threatening
chemotherapies: drug therapies designed to poison and kill cancer cells but spare normal cells
condom: a closed tube that covers the penis during sex, providing a barrier to semen and infectious agents such as bacteria and viruses
endometriosis: excessive buildup of the endometrial lining of the uterus
impotence: inability to sustain an erection
laparoscopy: a non-invasive surgical technique using cameras, specialized tools, and small incisions
ovarian cysts: fluid-filled swellings on the ovary
PAP smear: a screening test used to detect pre-cancerous and cancerous changes in the cervix due to human papillomavirus (HPV)
pelvic inflammatory disease (PID): an infection in the uterus and surrounding tissues; may result in scarring and/or infertility
radiation treatment: ionizing radiation directed at tumours to destroy cancer cells
safe sex: the use of a barrier, such as a condom, during sex to prevent transmission of infection
STD: a sexually transmitted disease caused by bacteria, fungus, or virus
The transmission of the disease does cause symptoms.
stem cell transplant: transplant of a donor's stem cells from sources such as bone marrow or umbilical cord blood; used to treat cancers of the blood and bone marrow
STI: sexually transmitted infection due to bacteria, fungus, or viruses; may not cause symptoms but is still contagious
surgery: performing an operation on a patient using instruments; in cancer, the removal of tumours and affected tissues
toxic shock syndrome: a rare, rapidly developing, and potentially fatal bacterial infection of the vagina; associated with extended tampon use
ultrasound: a medical diagnostic technique in which high-frequency sound waves are bounced off body structures to obtain an image
venereal: referencing the genitals or external sex organs
viral STIs: examples are HIV, HPV, and hepatitis; more problematic, possibly incurable because they cannot be treated with antibiotics
yeast infection: candidiasis; a common form of fungal infection of the vagina or penis; characterized by itch, redness, and discomfort
1.24. Lesson 6
Module 3—The Male and Female Reproductive Systems
Lesson 6—Male Hormones

© Niderlander/Dreamstime
 Get Focused
Get Focused
Being male is a process that starts with a chromosomal arrangement determined at fertilization, and is not complete until maturation happens in puberty. Being male means the chromosomal arrangement is an X and a Y chromosome. This chromosome arrangement then causes testosterone to start being produced. The secretion of testosterone causes the formation of the male genitalia of a fetus in utero (in the uterus). The right timing and the proper amount of testosterone produced helps mature the male reproductive system so that continuation of the species is possible.
José, from “A Fertility Case Study,” started going through puberty at 12 years of age. For boys, the age that puberty starts varies greatly, but is said to begin when gonadotropin releasing hormone (GnRH) production is increased by the hypothalamus. This hormone activates the anterior pituitary to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH), sometimes referred to in males as interstitial cell stimulating hormone (ICSH).
FSH stimulates sex organ development and gamete production, and leads to the Sertoli cells secreting inhibin. Inhibin targets the anterior pituitary and hypothalamus to inhibit FSH, creating a negative feedback loop.
LH or ICSH causes the interstitial cells in the testes to produce testosterone.
As José was going through puberty, both his primary and secondary sex characteristics were developing. The testosterone surge that occurred during puberty had an effect on his entire body. He developed facial and body hair, his voice deepened, his shoulders broadened, his hips narrowed, and he developed more muscle mass. However, by the time José was in high school and playing sports, he noticed that his muscle development was not as significant as the muscle development in some of the other players on his football team. He wondered about this difference.
In this lesson you will study the following focusing questions:
-
What are the male reproductive hormones?
-
How do hormones maintain in the male reproductive system?
-
What role do the male hormones play in regulating the primary and secondary sex characteristics?
gonadotropin releasing hormone (GnRH): a hormone produced by the hypothalamus; stimulates the anterior pituitary to produce FSH and LH
follicle-stimulating hormone (FSH): a hormone produced by the anterior pituitary; causes spermatogenesis in males
luteinizing hormone (LH): a reproductive hormone produced by the anterior pituitary; causes the release of testosterone in males, where it is also known as interstitial cell stimulating hormone (ICSH)
In females, LH triggers ovulation, stimulates the formation of the corpus luteum, and acts with FSH to stimulate estrogen production.
interstitial cell stimulating hormone (ICSH): also known, in the male, as luteinizing hormone
 Module 3: Lesson 6 Assignment
Module 3: Lesson 6 Assignment
Download a copy of the Module 3: Lesson 6 Assignment to your computer now. You will receive further instructions on how to complete this assignment later in the lesson.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
Make any notes about “A Fertility Case Study” from this lesson and place them in your course folder for your teacher’s feedback.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.25. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
Hormone control of the male reproductive system is important for proper sexual development and gamete production. As you do the following reading and view the video, you will better understand what happens when the male sex hormones are secreted, how the hormones control sexual development and gamete production, and what happens to the male reproductive system as aging occurs.
Depending on your learning style, you may choose to do the Read or the Watch and Listen; however, the Watch and Listen provides additional information on technologies and societal issues related to the course that you will find useful. It is an excellent idea to do both the Read and Watch and Listen.
You should make summary notes on the material that you will be reviewing and store this information in your course folder. Recall from Unit A that an excellent way to summarize hormone information is in the form of a feedback loop or a flow chart.
 Read
Read
By reading pages 492 up to “Hormonal Regulation of the Female Reproductive System” on page 495 of your textbook, you will review how the chromosomal sex of an individual is determined and how the male sex hormones cause male development of the embryo. You will advance your learning by reading about how the male reproductive system is further developed and matured in puberty, as well as about the changes that occur throughout the aging process.
 Watch and Listen
Watch and Listen
It is very important to understand the main periods of hormone production, the types of hormones produced, the function of each hormone, and how the hormones are regulated in the male body. To help you further develop a clear understanding of the hormone control of the male reproductive system, watch the following video.
“The Human Male Reproductive System: Perpetuating the Species” examines normal function and control of the male sex hormones. Watch the the following segments:
- “Regulation of Sperm Production”
- “Bio Review: Control of Testosterone Levels”
- “Testosterone Profile”
You may be required to enter a username and password to access the video. Contact your teacher for this information.
You may wish to add information according to your learning style to your course folder from the video.
 Discuss
Discuss
During the teen years, body development occurs differently for everyone. No two people develop at exactly the same rate or to the same proportions. This can often put pressure on individuals who are not developing as quickly as their peers.
Many high school athletes can perform as top athletes in more than one sport. This was exactly José’s situation when he was in high school. He was one of the top athletes on his high school's sports teams, but a few of the players were developing muscle mass much faster than him. José noticed that the coach did not say anything about their enhanced athletic ability and that the bigger players actually were getting more playing time. One day in the locker room he overhead a couple of the muscular athletes talk about the “juice” they were taking and how much it had helped them to be stronger athletes. They noticed that José had overheard their conversation and offered him some of the “juice.” They explained how it had helped them develop muscle mass.
anabolic steroids: male steroid hormones (including testosterone) that enhance muscle development
steroids: a group of lipids derived from cholesterol
All male and female sex hormones are steroids.
José decided to research the juice. Once he discovered that the juice was a mixture of anabolic steroids, he wanted to learn what he could about normal male hormone production and function so that he could compare this with the effects anabolic steroids would have on his body. Without knowing what the functions of normal male sex hormone secretions are and the effects that steroids can have, José could not make an informed choice about whether or not to take the “juice.” His research helped him understand the effects this “juice” can have on enhancing performance as well as the side effects of using steriods. José also discovered that the use of steroids by high school students was increasing.
In the discussion board you have access to, discuss one, a few, or all of the following questions. This work will help you with Part 2 of the module assessment.
D 1. What can happen if the production of a hormone is not regulated properly?
D 2. Have you ever encountered any pressure to “beef up,” meaning try anabolic steroids?
D 3. Do you think teens, such as yourself, fully understand the implications of using steroids?
D 4. Is having the “right” image of being male affecting young men today? If so, how?
 Self-Check
Self-Check
Test your understanding of the negative feedback control of the male sex hormones by correctly labelling the “Hormonal Control of the Male Reproductive System” diagram.
 Self-Check Answers
Self-Check Answers
-
hypothalamus
-
GnRH
-
LH
-
FSH
-
testis
-
interstitial cells produce testosterone
-
seminiferous tubules produce sperm and inhibin
1.26. Page 3
Module 3—The Male and Female Reproductive Systems
 Reflect and Connect
Reflect and Connect
Throughout all of life—even prior to birth and into old age—testosterone is being produced in the male reproductive system. There are times in a male’s life when testosterone levels peak. In the Lesson 6 Assignment you will see a visual representation of how testosterone levels fluctuate in the blood by completing a graphing exercise.
 Module 3: Lesson 6 Assignment
Module 3: Lesson 6 Assignment
Retrieve the copy of the Module 3: Lesson 6 Assignment that you saved to your computer earlier in this lesson. Complete the assignment. Save your completed assignment in your course folder. You will receive instructions later in this lesson about when to submit your assignment to your teacher.
 Reflect on the Big Picture
Reflect on the Big Picture
Update: A Fertility Case Study
For a young person and an athlete, there can be a lot of pressure to look a certain way or perform at a certain calibre. Accepting your own body image can be hard when you are bombarded with media images of what a “perfect” body looks like. The fame and fortune that can come with high-level athletic performance will only come as long as performance is at a peak. To maintain their ”image” and level of ”performance,” some individuals may feel the need to resort to the use of some of the 100 different varieties of anabolic steroids.
Even though José looked into normal male hormone production and control of the male reproductive system, as well as the risk factors associated with taking anabolic steroids, he decided to join his team mates and take the performance-enhancing drugs. His natural athletic ability, enhanced by the steroid use, allowed him to be selected for a professional sports team. Once on the team, he felt he needed to maintain his steroid use to keep up his performance and to keep his position on the team. This led to years of steroid use.
José kept this information from Maria, his wife, until he was diagnosed with low sperm count when they were attempting to start a family. He then discussed his steroid use with Maria and their fertility doctor. José explained that he slowly got off steroid use about a year ago and that he had used a variety of drugs that maintained his muscle mass and also counteracted the steroid affects.
Now that you have been informed of José’s history, take the time to make notes on this for “A Fertility Case Study” in the Unit B Assessment.
 Going Beyond
Going Beyond
Testosterone levels should be within a normal range in both men and women. However, disorders of the body may need to be treated with various types of steroids. The use of anabolic steroids can have many harmful effects, yet there are some body disorders that need treatment through the use of steroids. See if you can find out why steroids may be used to help treat individuals with HIV infection, Addison’s disease, arthritis, and many other disorders.
 Module 3: Lesson 6 Assignment
Module 3: Lesson 6 Assignment
Submit your completed Module 3: Lesson 6 Assignment to your teacher for assessment.
1.27. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In this lesson you considered the following focusing questions:
-
What are the male reproductive hormones?
-
How do hormones maintain homeostasis in the male reproductive system?
-
What role do the male hormones play in regulating the primary and secondary sex characteristics?
Although gender is first controlled by the chromosome arrangement received from our parents, it is hormones that lead to sexual development, gamete production, and the eventual continuation of the species.
Male hormone production begins in an embryo in the uterus. The process of sexual maturation happens during puberty, with the increase in production of GnRH from the hypothalamus. GnRH then causes the anterior pituitary to produce both FSH and LH. The production of FSH causes the testes to start producing sperm and the hormone inhibin, which feeds back negatively to the pituitary to control further production of FSH. While LH causes the testes to produce testosterone, high levels of the hormone provide a negative feedback control of the hypothalamus and pituitary to regulate LH production, thus also regulating testosterone production. Testosterone is responsible for the proper development and maturation of the primary and secondary sex characteristics.
Chemical hormone control of the mature male reproductive system causes a peak in testosterone levels during three major times in a male’s life: in utero, at birth, and during puberty. After puberty, testosterone levels stay at a steady rate for most of the remainder of a man’s life. Levels of testosterone can begin to drop at about age 40, a condition sometimes referred to as andropause. Although a male continues to produce testosterone throughout his life, sperm count is reduced as he ages.
Understanding the scientific effect of testosterone on the body has led to the technological production of synthetic anabolic steroids. Although steroids can sometimes be used to treat disorders, like naturally low testosterone levels (called hypogonadism), anabolic steroids affect society in a much greater way through their misuse. The desire to look or perform better may lead some individuals to misuse anabolic steroids, even when they are informed of the risk factors involved.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
anabolic steroids: male steroid hormones (including testosterone) that enhance muscle development
follicle-stimulating hormone (FSH): a hormone produced by the anterior pituitary; causes spermatogenesis in males
gonadotropin releasing hormone (GnRH): a hormone produced by the hypothalamus; stimulates the anterior pituitary to produce FSH and LH
interstitial cell stimulating hormone (ICSH): also known, in the male, as the luteinizing hormone
luteinizing hormone (LH): a reproductive hormone produced by the anterior pituitary; causes the release of testosterone in males, where it is also known as the interstitial cell stimulating hormone (ICSH)
In females, LH triggers ovulation, stimulates the formation of the corpus luteum, and acts with FSH to stimulate estrogen production.
steroids: a group of lipids derived from cholesterol
All male and female sex hormones are steroids.
1.28. Lesson 7
Module 3—The Male and Female Reproductive Systems
Lesson 7—Female Hormones
 Get Focused
Get Focused

© Monkey business Images/shutterstock
Although there is a lack of scientific understanding of the hormonal process that triggers an embryo to undergo female sexual development, there is a very good understanding of what happens during puberty, the menstrual cycle, and aging. Being female is designated by the chromosomal arrangement of two X chromosomes, which causes a female to develop female genitalia, begin having a menstrual cycle, and undergo menopause. The beginning of the menstrual cycle allows the female to fulfill her role in the continuation of the species.
The beginning of puberty is similar in men and women. The beginning of puberty is defined when the hypothalamus begins producing more gonadotropin releasing hormone (GnRH). GnRH then stimulates the anterior pituitary to start producing both follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH then act on the female gonads (the ovaries), to produce the female sex hormones estrogen and progesterone. Once estrogen and progesterone are secreted, they cause the maturation and development of the female primary and secondary sex characteristics and the start of the menstrual cycle.
When Jane, from Couple 1 in “A Fertility Case Study” was in high school, she was a competitive gymnast. Her skill level was very good and she was competing at the provincial and national level. In her Grade 11 year, Jane was 17, she was 5-foot-3 (1.6 m) and weighed 95 pounds (45 kg). What most people did not know was that Jane had an eating disorder, which she had battled since she was 10. Furthermore, at 17, she had not yet started menstruating. When she started training in Grade 12, she looked very fragile. Her coach was concerned about her well-being, and stopped her from competing in several early competitions and decreased her training by two-thirds. The coach shared his concerns with Jane's parents.
Jane discovered that when a woman of reproductive age is placed under physically demanding training regimes and the stress of competition, and has an eating disorder, her body may suffer from the absence of menstrual periods, called amenorrhea.
menstrual cycle: the female reproductive cycle of producing an egg and developing then shedding the endometrium every 28 days, on average
genitalia: external and internal sex organs
menopause: the period when menstruation and all female reproductive function ends; on average, at age 53
estrogen: a female steroid sex hormone secreted by the developing follicle prior to ovulation and the corpus luteum after ovulation
Estrogen develops the endometrium and female secondary sex characteristics.
progesterone: a female steroid sex hormone secreted by the corpus luteum after ovulation
Progesterone helps estrogen maintain the developed endometrium until menstruation.
amenorrhea: lack of menstruation due to low body fat, stress, or medical problems
Jane knew that she wanted children one day, so she decided to learn more about normal female reproductive hormone control and how her training and eating disorder were affecting her reproductive system. To understand what was happening to her body, she needed more information to make better decisions in her life now and in the future.
In this lesson you will examine the following focusing questions:
-
What are the female reproductive hormones?
-
How do hormones maintain homeostasis in the female reproductive system?
-
What role do the female hormones play in regulating primary and secondary sex characteristics?
 Module 3: Lesson 7 Assignment
Module 3: Lesson 7 Assignment
There is no assingment for this lesson.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
Make any notes about “A Fertility Case Study” from this lesson and place them in your course folder for your teacher’s feedback.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.29. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
To understand how the female reproductive system is controlled by hormones, complete the following readings and view the video. Remember to prepare summary notes, including labelled diagrams, flow charts, and feedback loops of the material you are learning. Store this information in your course folder.
 Read
Read
The hormonal control of the female reproductive system is much more complex than in the male reproductive system. Read pages 495 to 499 in the textbook, beginning at “Hormonal Regulation of the Female Reproductive System” to understand how puberty begins, the control of the menstrual cycle, and what happens at the end of the reproductive years in a female. Remember to make notes and illustrations to help you understand the secretion and control of the female sex hormones.
 Watch and Listen
Watch and Listen
Watch the video “Hormonal Controls and the Menstrual Cycle: The Renewal of Life.” The video compares the cyclical patterns of reproduction in humans with that of other mammals, and reviews the female reproductive structures and development of the secondary sex characteristics.
 Try This
Try This
Complete this drag-and-drop activity to determine whether you understand the functions of female sex hormones in the body.
 Discuss
Discuss
In the course discussion area, discuss one, a few, or all of the following questions.
D 1. When is a woman considered to be suffering from amenorrhea?
D 2. If a woman has very low levels of FSH and LH, how does this affect her reproductive system?
D 3. Should there be a minimum mass (weight) that female models and athletes need to meet in order to work professionally or compete?
D 4. Do you like the look of female body builders? Why or why not?
D 5. How important is it to you to have a properly functioning reproductive system?
1.30. Page 3
Module 3—The Male and Female Reproductive Systems
 Reflect on the Big Picture
Reflect on the Big Picture
Update: A Fertility Case Study
bone density: solidity of the bone; related to calcium intake, impact exercise, and blood estrogen levels
osteoporosis: the loss of bone density that increases risk of fracture
If osteoporosis occurs after menopause, the cause is often lack of estrogen.
Jane did more research on the hormonal control of the female reproductive system, and she found that bone density relates closely to menstrual regularity and the total number of menstrual cycles. Delayed onset of menstruation and/or premature cessation of menstruation removes estrogen’s protective effect on bone. Young women who experience delayed onset of menstruation and women who are no longer menstruating are more vulnerable to calcium loss, which results in a decrease in bone mass. Can you relate this fact to Jane’s appearance and develop a hypothesis to explain her frailty? Can this fact be related to the high frequency of osteoporosis in women in their menopausal years?
Once Jane understood the effects of the stress she was putting on her body, she sought help for her eating disorder and quit competing in gymnastics. In her early twenties she started having a normal menstrual cycle.
1.31. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In this lesson, you considered the following focusing questions:
-
What are the female reproductive hormones?
-
How do hormones maintain homeostasis in the female reproductive system?
-
What role do the female hormones play in regulating the primary and secondary sex characteristics?
To be able to perpetuate the species, females need to menstruate for their sexual hormones to be properly controlled. The proper control of the sexual hormones leads to a healthy reproductive system and a greater chance of having offspring.
For women, puberty starts with the increase in GnRH, which then causes the pituitary to release FSH and LH hormones. These hormones help with sexual development, successful formation of functioning gametes, and continued occurrence of the menstrual cycle.
Stress, eating disorders, and excessive exercise can play a major role in hormone function that can result in not having a proper menstrual cycle.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
amenorrhea: lack of menstruation due to low body fat, stress, or medical problems
bone density: solidity of the bone; related to calcium intake, impact exercise, and blood estrogen levels
estrogen: a female steroid sex hormone secreted by the developing follicle prior to ovulation and the corpus luteum after ovulation
Estrogen develops the endometrium and female secondary sex characteristics.
genitalia: external and internal sex organs
menopause: the period when menstruation and all female reproductive function ends; on average, at age 53
menstrual cycle: the female reproductive cycle of producing an egg and developing then shedding the endometrium every 28 days, on average
osteoporosis: the loss of bone density that increases risk of fracture
If osteoporosis occurs after menopause, the cause is often lack of estrogen.
progesterone: a female steroid sex hormone secreted by the corpus luteum after ovulation
Progesteron helps estrogen maintain the developed endometrium until menstruation.
1.32. Lesson 8
Module 3—The Male and Female Reproductive Systems
Lesson 8—Phases of Menstruation

© Alberto L. Pomares G./iStockphoto
 Get Focused
Get Focused
The beginning of menstruation represents the beginning of a female’s reproductive years. The start of the menstrual cycle is generally considered the pivotal event of puberty for females, and it indicates the time from which a female can conceive. The ability to be fertile means the ability to have offspring and, therefore, the ability to help in the continuation of the species.
ovarian cycle: the 28-day cycle of ovum development, in the following order: primary follicle, developing and mature follicle, ovulation of the egg, formation of the corpus luteum, and disintegration of the corpus luteum
uterine cycle: the 28-day cycle of shedding of the old endometrium (menstruation) and development of a new one
primary oocyte: the egg that the follicle is developing in the follicular phase, which has not completed the first meiotic division
The menstrual cycle is said to begin on the first day of bleeding and is usually a 28 day cycle. Both the ovarian and uterine cycles begin on this day. The ovarian cycle, which takes place in the ovaries, is divided into the follicular stage and the luteal stage. During the follicular stage, levels of FSH are high while stimulating normally one follicle to mature. The maturing follicle releases the ovarian hormones estrogen and progesterone. Estrogen then negatively feeds back to the pituitary to cause a reduction in the release of FSH. Estrogen also causes the hypothalamus to secret GnRH, which then leads to an increase in the pituitary hormone of LH. LH activates ovulation of the primary oocyte from the follicle.
follicular stage: the first 14 days of the menstrual cycle in which the follicle is developing a mature ovum for ovulation and the endometrium is building in preparation for implantation of a possible embryo
luteal stage: the period of the menstrual cycle after ovulation (days 15 to 28), when the old follicle forms a corpus luteum that secretes progesterone and estrogen to maintain the endometrium
The end of ovulation is considered the end of the follicular stage and the start of the luteal stage. With the release of the egg, the follicle develops into the corpus luteum under the influence of LH. Both ovarian hormones are secreted from the corpus luteum and their increased levels feedback negatively to the anterior pituitary to inhibit production of FSH and LH. As the corpus luteum disintegrates, the ovarian hormone levels decrease in the blood. The low blood levels of progesterone and estrogen are detected by the anterior pituitary and cause an increase in FSH and LH; the cycle starts again.
endometrium: the lining of the uterus that is developed under the influence of estrogen from days 1 to 14, becoming thick and engorged with blood to accept an implanting embryo should fertilization take place
On the first day of menstrual flow, the corpus luteum degeneration causes estrogen and progesterone to be at low levels in the blood. Estrogen blood levels begin to rise as a new follicle begins to mature, releasing the ovarian hormone. When estrogen levels are high, it causes the endometrium to thicken. A more rapid thickening of the endometrium lining occurs once the corpus luteum begins to produce progesterone, after ovulation has occurred. If fertilization takes place, the zygote travels through the oviduct and implants in the freshly, blood-engorged endometrial lining of the uterus. If fertilization does not occur, there is a disintegration of the endometrium lining, and it is expelled from the body during menstruation.
Without this intricate dance of pituitary and ovarian hormones, the menstrual cycle would not take place, and there would be no possibility of fertilization.
menopause: the end of ovulation and menstruation and the fading of secondary sex characteristics as estrogen and progesterone are no longer produced
hot flashes: periods of intense heat and sweating that occur as estrogen and progesterone hormone levels fluctuate during the years of menopause
hormone replacement therapy: combinations of estrogen and progesterone prescribed to decrease hot flashes and other discomforts that may come with menopause
As women age, the number of functioning follicular cells decreases, resulting in reduced production of estrogen and progesterone. The menstrual cycle becomes irregular and eventually ceases. This is called menopause, a period when the homeostasis of many hormones is interrupted, often resulting in the symptom of hot flashes.
Hormone replacement therapy can be used to treat some of the symptoms of menopause, however, there are several possible side effects, such as the increased possibility of breast cancer, heart attack, stroke, and blood clots.
Just because a female begins menstruation does not mean that she is limited to doing only certain activities or that there is a clear and easy path to fertilization. As you have been learning, there are many, many obstacles to fertilization and the birth of a healthy child.
In the role of fertility doctor, you have identified that Maria suffers from dysmenorrhea and Jane from amenorrhea. To understand her disorder, each woman needed to learn more about the structure and function of a healthy, properly functioning reproductive system, which includes a regular menstrual cycle. Understanding the “normal” function of the reproductive system helped them to understand the disorders from which they were suffering, as well as the choice of treatment options that were available to them.
In addition to menstrual problems, a clear understanding of the menstrual cycle helps you understand when fertility can and cannot happen. This understanding is important for both men and women in family planning and prevention of unplanned or unexpected pregnancies.
In this lesson you will study the events of the menstrual cycle, how hormones control the cycle of menstrual events, and where the cycle occurs in the female life cycle. You will consider the following focusing questions:
-
What are the physiological events of menstruation?
-
What hormone(s) control the specific events of menstruation?
-
When does menstruation naturally begin and end?
 Module 3: Lesson 8 Assignment
Module 3: Lesson 8 Assignment
Download a copy of the Module 3: Lesson 8 Assignment to your computer now. You will receive further instructions on how to complete this assignment later in the lesson.
In addition to the lesson work you complete for your course folder, you answer assignment questions based on how the pituitary and ovarian hormones control and are controlled by the events of the menstrual cycle.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
Make any notes about “A Fertility Case Study” from this lesson and place them in your course folder for your teacher’s feedback.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.33. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
To understand the hormonal control of the female reproductive system, it is recommended to first do the reading and then watch the video segments. It is recommended that you make your own notes, particularly in the form of a flow chart or concept map as well as a feedback loop illustrating the menstrual cycle. The feedback loop is an essential tool in understanding the events of the menstrual cycle. Store your work in your course folder for later review.
 Read
Read
To understand the regulation of the menstrual cycle, read pages 495 to 499 in the textbook, starting with the section titled “Sex Hormones and the Female Reproductive System” through to the “Summary.”
 Watch and Listen
Watch and Listen
It is hard to separate female sex hormones from the menstrual cycle, so for the best understanding of the menstrual cycle, it is recommended that you view the entire video “Hormonal Controls and the Menstrual Cycle: The Renewal of Life” video. You have already seen this video in Lesson 7, but reviewing this material will help you integrate the information. You may be required to enter a username and password in order to access the video. Contact your teacher for this information.
In Unit A you learned how to draw feedback loops. You may find that preparing a feedback loop of the events of the menstrual cycle helps you understand the events in the correct sequence. Check your work with your teacher.
 Self-Check
Self-Check
The reading and video examine how the menstrual cycle is controlled by hormones. Test your understanding of hormonal control of the ovarian cycle by correctly labelling the following images.
SC 1. Provide labels for the following diagram, which shows the hormonal control of the ovarian cycle. Outline the steps involved in this flow chart.
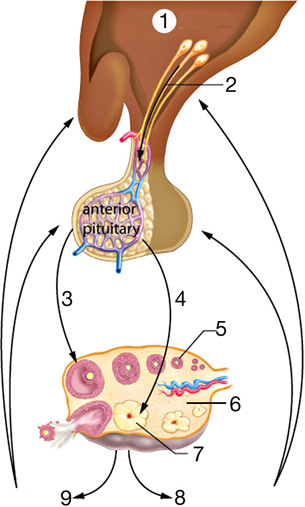
Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 496, fig. 14.15 Reproduced by permission.
SC 2: Provide labels for the following diagram, which shows the the ovarian cycle. Outline the steps involved in this flow chart.

Inquiry into Biology (Whitby, ON: McGraw-Hill Ryerson, 2007), 496, fig. 14.14 Reproduced by permission.
 Self-Check Answers
Self-Check Answers
SC 1. Hormonal Control of the Ovarian Cycle
- hypothalamus
- GnRH
- LH
- FSH
- follicle
- ovary
- corpus luteum
- progesterone
- estrogen
The hypothalamus produces gonadotropin releasing hormone (GnRH), which stimulates the anterior pituitary to produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH stimulates the follicle to produce estrogen. LH stimulates the corpus luteum to produce progesterone.
SC 2. The Ovarian Cycle
- ovary
- oviduct
- uterus
- vagina
- developing follicles
- mature follicle
- ovum
- ovum released
- corpus luteum
- degenerating corpus luteum
- corpus albicans
- blood vessels
- immature follicles
A follicle matures by growing layers of follicular cells and a central fluid-filled vesicle. The vesicle contains the maturing ovum. At ovulation, the follicle ruptures and the ovum is released into the oviduct. The follicle develops into a corpus luteum. If pregnancy does not occur, the corpus luteum starts to degenerate after about 10 days. Note that the follicle does not migrate around the ovary, as shown here for clarity, but goes through all the stages in one place.
 Module 3: Lesson 8 Assignment
Module 3: Lesson 8 Assignment
Retrieve the copy of the Module 3: Lesson 3 Assignment that you saved to your computer earlier in this lesson. Complete the assignment. Save your completed assignment in your course folder. You will receive instructions later in this lesson about when to submit your assignment to your teacher.
 Discuss
Discuss
In the course discussion area, discuss one, a few, or all of the following questions.
D 1. What are medication-free ways of helping to have a pain free and/or regular menstrual cycle?
D 2. Why do females who live together often have menstrual cycles that happen at the same time?
1.34. Page 3
Module 3—The Male and Female Reproductive Systems
 Reflect on the Big Picture
Reflect on the Big Picture
Update: A Fertility Case Study
Reflection on “A Fertility Case Study” shows that both Maria and Jane had specific menstrual cycle disorders. Jane was not given any specific medications, but was able to sort through her condition (amenorrhea) by understanding the menstrual cycle, getting help with her eating disorder, and reducing her stress/training schedule.
Maria’s condition of dysmenorrhea was treated by her going on a birth-control pill, which alleviated her painful menstrual cramps and kept her on a very regular menstrual cycle. She stayed on the pill for 12 years until she and José were ready to have a family.
As the women's fertility doctor, make sure you record their sexual health history. Sexual health history is needed to understand present fertility problems.
 Going Beyond
Going Beyond
There are as many differences in menstrual cycles as there are females in the world. Take some time now to do some research on common menstrual disorders such as menorrhagia, hypomenorrhea, polymenorrhea, and oligomenorrhea.
See if you can find what the difference is, specifically related to hormone control, between an estrus and a menstrual cycle.
 Module 3: Lesson 8 Assignment
Module 3: Lesson 8 Assignment
Submit your completed Module 3: Lesson 8 Assignment to your teacher for assessment.
1.35. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
You have considered the following focusing questions:
-
What are the physiological events of menstruation?
-
What hormone(s) control the specific events of menstruation?
-
When does menstruation naturally begin and end?
pituitary hormones: FSH and LH secreted from the anterior pituitary
ovarian hormones: estrogen secreted from the pre-ovulatory follicle and estrogen/progesterone secreted from the corpus luteum
Sexual maturation in females occurs with the onset of puberty. Puberty begins when GnRH is released from the hypothalamus and acts on the anterior pituitary to produce the reproductive pituitary hormones of FSH and LH. FSH and LH then activate the female gonads, the ovaries, to produce the ovarian hormones, progesterone and estrogen, throughout the course of the ovarian and uterine events of the menstrual cycle.
The maturation of the ovum, or egg, and the preparation of the uterine lining for implantation of the zygote are regulated and achieved by the events of the menstrual cycle. The production levels of reproductive hormones drops as women age, resulting in the onset of menopause.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
endometrium: the lining of the uterus that is developed under the influence of estrogen from days 1 to 14, becoming thick and engorged with blood to accept an implanting embryo should fertilization take place
follicular stage: the first 14 days of the menstrual cycle in which the follicle is developing a mature ovum for ovulation and the endometrium is building in preparation for implantation of a possible embryo
hormone replacement therapy: combinations of estrogen and progesterone prescribed to decrease hot flashes and other discomforts that may come with menopause
hot flashes: periods of intense heat and sweating that occur as estrogen and progesterone hormone levels fluctuate during the years of menopause
luteal stage: the period of the menstrual cycle after ovulation (days 15 to 28), when the old follicle forms a corpus luteum that secretes progesterone and estrogen to maintain the endometrium
menopause: the end of ovulation and menstruation and the fading of secondary sex characteristics as estrogen and progesterone are no longer produced
ovarian cycle: the 28-day cycle of ovum development, in the following order: primary follicle, developing and mature follicle, ovulation of the egg, formation of the corpus luteum, and disintegration of the corpus luteum
ovarian hormones: estrogen secreted from the pre-ovulatory follicle and estrogen/progesterone secreted from the corpus luteum
pituitary hormones: FSH and LH secreted from the anterior pituitary
primary oocyte: the egg that the follicle is developing in the follicular phase, which has not completed the first meiotic division
uterine cycle: the 28-day cycle of shedding of the old endometrium (menstruation) and development of a new one
1.36. Lesson 9
Module 3—The Male and Female Reproductive Systems
Lesson 9—Medical Use of Reproductive Hormones
 Get Focused
Get Focused

© 2008 Jupiterimages Corporation
Without proper hormonal control of the reproductive system, events like ovulation and sperm production cannot take place. This can result in the lack of fertilization and the failure to ensure continuation of the species. Normal hormone control may be altered knowingly by taking hormones to enhance or prevent pregnancy and to treat disorders. Hormone control may also be altered unknowingly through the effects of endocrine disruptors.
endocrine disruptor: a chemical capable of disrupting hormone function
In reproduction, the term refers to man-made or natural chemicals found in the environment that have unintended negative effects on the reproductive tract, ranging from infertility to cancer.
Endocrine disruptors are synthetic or naturally occurring substances that interfere with the functioning of the body’s normal production of hormones. The endocrine disruptors can be absorbed into the body through contaminated water, food, or air. Their effects can halt or stimulate normal hormone levels, or they may change how hormones travel in the body. The hormone feedback loop can be altered. Some known human endocrine disruptors are dioxin, PCBs, DDT, and diethylstilbesterol (a drug known as DES). Research has found that DES, a synthetic estrogen that was used to prevent miscarriages, often led to increased cervical cancer, birth defects of the uterus and ovaries, and suppression of the immune system in daughters of women who used DES.
Any time the normal release of reproductive hormones is changed, there are consequences. For example, when the release of FSH and LH is affected, the result is a reduced development of egg and sperm. Progestin, synthetic progesterone, was the first chemical used as a female oral contraceptive, known as “the pill.” Varying quantities of estrogen and progesterone are used in today’s contraceptive pills.
Other conditions can be treated with sex hormones. In the initial treatments using chemotherapy, prostate cancer was treated with female sex hormones. Many types of cancer are now treated with female and male sex hormones. Menopause, andropause, impotence, low sperm count, arthritis, and osteoporosis can be treated through the use of sex hormones.
Exposure to endocrine disruptors during development can have permanent effects on an organism. There is further evidence that endocrine disruptors may have consequences for many generations, not just for the immediate person or organism.
Remembering back to “A Fertility Case Study,” both José and Maria had hormone issues associated with their infertility problems. Maria used oral contraceptives for a long time prior to wanting to start a family, and José had misused anabolic steroids for many years.
Understanding how normal reproductive hormones control and affect the body can help you understand how these reproductive hormones are used to promote or reduce conception potential, to treat diseases, and how they are influenced by endocrine disruptors.
Keep the following focusing question in mind as you work through this lesson:
-
What are the various effects of reproductive hormones?
© Dianne Maire/shutterstock
 Module 3: Lesson 9 Assignment
Module 3: Lesson 9 Assignment
Download a copy of the Module 3: Lesson 9 Assignment to your computer now. You will receive further instructions about how to complete this assignment later in the lesson.
In addition to the lesson work you complete for your course folder, you will complete questions on endocrine disruptors in the environment for assessment.
You must decide what to do with the questions that are not marked by the teacher.
Remember that these questions provide you with the practice and feedback that you need to successfully complete this course. You should respond to all of the questions and place those answers in your course folder.
Make any notes about “A Fertility Case Study” from this lesson and place them in your course folder for your teacher’s feedback.
Remember that you also have the option of trying additional questions from the textbook for further practice. Consult with your teacher for the answers to these questions. The Key will also provide you with many Diploma Exam-style multiple-choice, numerical-response, and written-response questions that will be an excellent review of the module. Practising your responses to these types of questions is good preparation for the Diploma Exam.
1.37. Page 2
Module 3—The Male and Female Reproductive Systems
 Explore
Explore
Before beginning the material in this lesson, ensure that you understand the normal reproductive hormones that control in both the male and female reproductive systems. As a review, you may want to go back over pages 492 to 499 of the textbook. You may choose to do the questions on page 502 of your textbook and discuss your responses with your teacher.
 Read
Read
To learn about endocrine disruptors, read page 501 of the textbook. Conduct an Internet search using the search terms “endocrine disruptors” to gain further understanding of what they are, where they are found, and what effects they have on animals and humans.
 Watch and Listen
Watch and Listen
View the following animation and video about how an endocrine disruptor works.
 Module 3: Lesson 9 Assignment
Module 3: Lesson 9 Assignment
Complete the following online assignment and the two questions in “Endocrine Disruptors in the Environment” from page 501 of the textbook. Place all of your answers in the copy of Module 3: Lesson 9 Assignment that you saved to your computer earlier in this lesson. Save your completed assignment in your course folder. You will receive instructions later in this lesson on when to submit your assignment to your teacher.
 Discuss
Discuss
Through your course discussion area, share your thoughts on one, a few, or all of the following questions.
D 1. Do you feel that oral contraceptives are safe to take?
D 2. How well do you think governments control-test for endocrine disruptors in products that we use?
D 3. Do you think that your age group is sufficiently informed about endocrine disruptors?
D 4. How can we, as a society, break away from our overabundant use of soft plastics?
D 5. Did Canada make a wise decision to ban Bisphenol A?
D 6. Should we look at animal studies to determine how chemicals can affect humans?
1.38. Page 3
Module 3—The Male and Female Reproductive Systems
 Reflect and Connect
Reflect and Connect
This module has examined how the normal human sexual reproductive hormone pathways work. Reproductive hormones are used to help or prevent reproductive potential. They are also used to treat various diseases.
For humans, particularly the animal kingdom as a whole, there is a constant bombardment of chemicals infiltrating our environments. How these chemicals influence normal hormone control is just beginning to be understood. Endocrine disruptors are an issue of growing importance in the concern and desire to maintain healthy lifestyles for many organisms. Observation of other organisms sheds light on how these chemicals may affect our own human endocrine pathways.
 Reflect on the Big Picture
Reflect on the Big Picture
As scientists and researchers gain further understanding of how endocrine disruptors affect wildlife, more information is also gained on how these chemicals can affect human populations. Could these chemicals be causing some of the infertility problems that are seen in North America today?
Update: A Fertility Case Study
From “A Fertility Case Study,” you have seen that Maria was on oral contraceptives for a long time. As her fertility doctor, you first put Maria on Provera, cyclic progestin to regulate her cycle. This medication mimics the second half of her menstrual cycle. Next, like José, she is prescribed Clomid. This drug makes her more likely to ovulate each month. The treatment you have prescribed for both Maria and José are well-established treatments using the most widely used fertility drugs.
In this module you have examined some of the structural, functional, and hormonal issues that could affect the fertility of each of the couples in the case study. In the next module you will examine the events from conception to birth. The nine-month path can involve many situations affecting the successful birth. You may find additional reasons to explain the fertility issues of the couples as you work through Module 4.
 Going Beyond
Going Beyond
Complete one of the following options.
Option 1: Take a closer look at any one of the known endocrine disruptors mentioned at the beginning of this lesson and do further research on how this chemical directly affects humans.
Option 2: Propose and defend a position related to mandatory contraception and a developing nation’s concern with overpopulation and teenage pregnancy.
Option 3: Using the search terms “CBC,” “documentaries,” and “The Disappearing Male,” you will be able to access the video “The Disappearing Male.” As you watch, consider the following questions. You may share your answers on the discussion board or with your teacher.
-
Provide three examples from the growing body of evidence that male sexual health is declining.
-
How many man-made chemicals have been created in the past 60 years?
-
What is the purpose of the chemical Bisphenol A?
-
What is the purpose of the class of chemicals known as phthalates?
-
What is the current World Health Organization standard for determining male fertility?
-
What three characteristics are used to measure sperm quality?
- What group of chemicals has the ability to alter the development of testes?
-
What is the source of most modern day synthetic chemicals?
-
What city is home to approximately 40% of the Canadian chemical industry?
-
What factor is declining in twenty of the world’s most industrialized countries?
-
What common chemical is found in hospital nursery wards and is considered to be a reproductive toxicant?
-
What chemical that has been around since 1891 is raising the most concern today?
-
What natural human hormone does Bisphenol A mimic?
-
Males who have undescended testicles are times more at risk to develop testicular cancer.
-
Why did Canada take the unprecedented step of banning Bisphenol A from baby bottles?
 Module 3: Lesson 9 Assignment
Module 3: Lesson 9 Assignment
Submit your completed Module 3: Lesson 9 Assignment to your teacher for assessment.
1.39. Page 4
Module 3—The Male and Female Reproductive Systems
 Lesson Summary
Lesson Summary
In this lesson you considered the following focusing question:
-
What are the various effects of reproductive hormones?
As a species we have managed to be able to control most aspects of our reproduction. Much of this control has come through major tinkering with our reproductive hormones. Hormones are used to prevent and assist pregnancies. Reproductive hormones are used in the treatment of conditions such as cancer and arthritis. Many chemicals that are used in products that promote improvement in our daily lives are now being identified as affecting our endocrine systems. Evidence now supports that the use of reproductive hormones, although beneficial to us at times, is not only having adverse effects on human health, but is having an affect on many other organisms as well.
Lesson Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
encodrine disruptor: a chemical capable of disrupting hormone function
In reproduction, the term refers to man-made or natural chemicals found in the environment that have unintended negative effects on the reproductive tract, ranging from infertility to cancer.
1.40. Module Summary/Assessment
Module 3—The Male and Female Reproductive Systems
 Module 3 Summary
Module 3 Summary
This module focused on the male and female reproductive systems and on the hormones impacting reproduction. You were asked to consider the following inquiry questions:
-
What are the structures of the male and female reproductive systems, and how do these structures function, to ensure the survival of the human species through reproduction?
-
How is the homeostasis of reproduction maintained by hormones in the male and female?
This module began with a study of human reproduction and the structures and functions of the male and female systems. The information presented in the lessons has helped you assess the importance of your reproductive health. As you head into your reproductive years, it is important to learn the structures and function of the male and female reproductive systems and how each system forms functional gametes. Making choices that maintain your sexual health are vital for who you are now and your plans for a future family. By understanding how sexually transmitted diseases can affect your reproductive system and society as a whole, you are better informed to make healthy choices. Examining reproductive technologies will help you understand how infertility issues can be addressed and the ethical issues that you will have to consider as a member of society.
From the study of this module, you will have gained an understanding of the chemical control that governs human reproductive systems. You will have come to comprehend the importance of how hormones control the various events and cycles of human reproduction. Whether you are male or female, it is tempting and sometimes necessary to use technology to help maintain a balance of reproductive hormones to help with various effects on the body. Knowing the effects that reproductive hormones have on your reproductive system will help you make the best choices possible for maintaining your reproductive health. The understanding of how chemistry controls the various stages and phases of reproductive hormone control is important during puberty and later in life during the aging process.
Before you begin the Module 3 Assessment, you may decide to complete some of the review questions on pages 504 to 505 in your textbook.
Your teacher can suggest to you which questions might meet your needs and provide you with feedback about your responses.
Module Assessment
You must complete both Part 1 and Part 2 of the Module 3 Assessment.
1.41. Module Glossary
Module 3—The Male and Female Reproductive Systems
Module Glossary
Consult the glossary in the textbook for other definitions that you may need to complete your work.
abstinence: not having sexual intercourse
amenorrhea: lack of menstruation due to low body fat, stress, or medical problems
anabolic steroids: male steroid hormones (including testosterone) that enhance muscle development
androgens: male group of steroid hormones; includes testosterone
antibodies: blood proteins that bind to and destroy infectious antigens such as bacteria and viruses
asymptomatic infection: infection that is present but the affected person does not experience symptoms
bacterial STIs: examples are gonorrhea, syphilis, and chlamydia; can be treated with antibiotics
body fluids: primarily semen, vaginal fluid, saliva, and blood
bone density: solidity of the bone; related to calcium intake, impact exercise, and blood estrogen levels
bone marrow transplant: a procedure in which bone marrow from a donor is used to “seed” new bone marrow in blood and bone marrow cancer patients
cancer: uncontrolled cell division resulting in tumours that may be life-threatening
cervix: the tightly constricted opening from the vagina into the uterus
chemotherapies: drug therapies designed to poison and kill cancer cells but spare normal cells
condom: a closed tube that covers the penis during sex, providing a barrier to semen and infectious agents such as bacteria and viruses
corpus luteum: the structure that develops from a matured follicle that has released its egg
The corpus luteum produces progesterone and some estrogen. If pregnancy does not occur, the corpus luteum degenerates.
Cowper’s gland: a gland secreting fluids to form semen
ductus deferens: a smooth muscle tube that carries the semen from the epididymis to the penis
dysmenorrhea: severe menstrual cramps
egg [ovum (singular), ova (plural), oocyte]: the female gamete that contributes half of the chromosomes to the zygote in sexual reproduction
ejaculation: the release of semen from the penis
ejaculatory duct: a tube from the ductus deferens to the penis
embryo: the offspring in the period of development from the cleavage of the zygote to the ninth week, when the embryo becomes a fetus
encodrine disruptor: a chemical capable of disrupting hormone function
In reproduction, the term refers to man-made or natural chemicals found in the environment that have unintended negative effects on the reproductive tract, ranging from infertility to cancer.
endometrial lining: the lining of the uterus that is thickened monthly to allow implantation of an embryo, and is shed in menstruation if fertilization does not occur
endometriosis: excessive buildup of the endometrial lining of the uterus
endometrium: the lining of the uterus that is developed under the influence of estrogen from days 1 to 14, becoming thick and engorged with blood to accept an implanting embryo should fertilization take place
epididymis: a cap on each testicle where sperm are matured and stored prior to ejaculation
estrogen: a female steroid sex hormone secreted by the developing follicle prior to ovulation and the corpus luteum after ovulation
Estrogen develops the endometrium and female secondary sex characteristics.
fertility: the ability to produce gametes and reproduce
fimbriae: finger-like projections that sweep the ovulated ovum into the oviduct
follicles: specialized cells that surround and nurture the developing ova in the ovary and that secrete estrogen and progesterone
follicle-stimulating hormone (FSH): a hormone produced by the anterior pituitary; causes spermatogenesis in males
follicular stage: the first 14 days of the menstrual cycle in which the follicle is developing a mature ovum for ovulation and the endometrium is building in preparation for implantation of a possible embryo
fraternal (dizygotic) twins: twins produced when two different eggs are fertilized by two different sperm; not identical and may be of different genders
gamete: a haploid cell made during meiosis that participates in fertilization to make a zygote
gametogenesis: the process of creating gametes from somatic cells; includes meiosis
gender: the sex of an organism
genitalia: external and internal sex organs
gestation: the period of pregnancy
gonadotropin releasing hormone (GnRH): a hormone produced by the hypothalamus; stimulates the anterior pituitary to produce FSH and LH
gonads: sex organs that produce gametes (sperm or egg); testes in males and ovaries in females
hormone replacement therapy: combinations of estrogen and progesterone prescribed to decrease hot flashes and other discomforts that may come with menopause
hot flashes: periods of intense heat and sweating that occur as estrogen and progesterone hormone levels fluctuate during the years of menopause
impotence: inability to sustain an erection
infertility: the inability to reproduce
inhibin: a hormone produced by Sertoli cells during spermatogenesis that inhibits GnRH, preventing excessive sperm production
interstitial cells: tightly packed testosterone-secreting cells that surround the seminiferous tubules in the testes
interstitial cell stimulating hormone (ICSH): also known, in the male, as the luteinizing hormone
laparoscopy: a non-invasive surgical technique using cameras, specialized tools, and small incisions
luteal stage: the period of the menstrual cycle after ovulation (days 15 to 28), when the old follicle forms a corpus luteum that secretes progesterone and estrogen to maintain the endometrium
luteinizing hormone (LH): a reproductive hormone produced by the anterior pituitary; causes the release of testosterone in males, where it is also known as the interstitial cell stimulating hormone (ICSH)
In females, LH triggers ovulation, stimulates the formation of the corpus luteum, and acts with FSH to stimulate estrogen production.
menarche: a female’s first menstrual cycle
menopause: the time in a woman’s life, at approximately age 50, when the production of estrogen and progesterone decreases, resulting in the cessation of menstrual cycles, reproductive function, and limited loss of secondary sex characteristics
menstrual cycle: the female reproductive cycle of producing an egg and developing then shedding the endometrium every 28 days, on average
menstruation: the monthly shedding of the endometrial lining
oligospermia (oligozoospermia): a condition in which there are less than 20 million spermatozoa per millilitre of semen
oocytes: cells that are undergoing meiosis in the ovary
oogenesis: the process of egg production in females
oogonia: diploid cells in the ovary that will undergo meiosis
osteoporosis: the loss of bone density that increases risk of fracture
If osteoporosis occurs after menopause, the cause is often lack of estrogen.
ovarian cycle: the 28-day cycle of ovum development, in the following order: primary follicle, developing and mature follicle, ovulation of the egg, formation of the corpus luteum, and disintegration of the corpus luteum
ovarian cysts: fluid-filled swellings on the ovary
ovarian hormones: estrogen secreted from the pre-ovulatory follicle and estrogen/progesterone secreted from the corpus luteum
ovaries: the paired female gonads that produce eggs and secrete progesterone and estrogen hormones
oviduct (Fallopian tube): the cilia-lined tube of smooth muscle that carries the ovulated egg from each ovary to the uterus
ovulation: the release of the mature ovum from the follicle of the ovary into the oviduct
PAP smear: a screening test used to detect pre-cancerous and cancerous changes in the cervix due to human papillomavirus (HPV)
pituitary hormones: FSH and LH secreted from the anterior pituitary
primary oocytes: the two cells produced prenatally by the mitotic division of the diploid oogonium
Primary oocytes remain at the meiotic prophase 1 stage of oogenesis until the female reaches puberty.
primary sex characteristics: structures in the male or female that are essential for reproduction
progesterone: a female steroid sex hormone secreted by the corpus luteum after ovulation
Progesterone helps estrogen maintain the developed endometrium until menstruation.
prostate gland: a muscle-like gland secreting alkaline fluid to neutralize the acids in urine
puberty: the period when reproductive abilities begin
radiation treatment: ionizing radiation directed at tumours to destroy cancer cells
safe sex: the use of a barrier, such as a condom, during sex to prevent transmission of infection
scrotum: a pouch of skin located below the penis that holds the testes
secondary sex characteristics: characteristics that distinguish male from female but are not required for reproduction
semen: the ejaculated liquid that contains sperm plus the secretions of the seminal vesicles, prostate, and Cowper’s gland
seminal vesicles: glands producing a fluid containing fructose, which supplies energy for use by sperm
seminiferous tubules: coiled, hollow tubes in the testes where sperm are produced
Sertoli cells: ‘nurse’ cells in the seminiferous tubules that assist in spermatogenesis and produce the hormone inhibin
sex characteristics: structures and characteristics that differentiate one gender from the other
sex chromosomes: the twenty-third pair of chromosomes that determines gender
XX is female, XY is male.
sex hormone: a biochemical compound controlling the development, maintenance, and function of the reproductive system and secondary sex characteristics
somatic cell: a normal diploid body cell; a cell not involved in fertilization
sperm: the male gamete
In sexual reproduction, the haploid sperm contributes half the chromosomes to the zygote; the egg contributes the other half.
spermatogenesis: the process of sperm production in males
spermatozoa: mature sperm stored in the epididymis
STD: a sexually transmitted disease caused by bacteria, fungus, or virus
All male and female sex hormones are steroids.
stem cell transplant: transplant of a donor’s stem cells from sources such as bone marrow or umbilical cord blood; used to treat cancers of the blood and bone marrow
STI: sexually transmitted infection due to bacteria, fungus, or viruses; may not cause symptoms but is still contagious
surgery: performing an operation on a patient using instruments; in cancer, the removal of tumours and affected tissues
testes: paired male gonads that produce sperm and secrete testosterone
testicles: a pair of male gonads producing sperm and testosterone; also called testes
testis determining factor (TDF): a protein produced by a gene on the Y chromosome, which results in male primary sex characteristics
testosterone: male sex hormone secreted by interstitial cells of the testes; results in male primary and secondary sex characteristics
toxic shock syndrome: a rare, rapidly developing, and potentially fatal bacterial infection of the vagina; associated with extended tampon use
ultrasound: a medical diagnostic technique in which high-frequency sound waves are bounced off body structures to obtain an image
urethra: the tube leading from the bladder to the penis
The urethra may carry either urine or semen.
uterine cycle: the 28-day cycle of shedding of the old endometrium (menstruation) and development of a new one
uterus: the reproductive organ in which embryonic and fetal development occurs
vagina: the muscular tube that leads from the uterus to the external environment
venereal: referencing the genitals or external sex organs
viral STIs: examples are HIV, HPV, and hepatitis; more problematic, possibly incurable because they cannot be treated with antibiotics
vulva: the external female genital organs